Table of Contents
Overview – Alcohol
Alcohol is a widely consumed psychoactive substance that modulates inhibitory and excitatory neurotransmission, stimulates the dopamine reward pathway, and contributes to significant global morbidity and mortality. In clinical practice, alcohol misuse is frequently encountered and implicated in a wide range of physical, psychiatric, and social issues. This article reviews alcohol’s neurobiology, health effects, dependence criteria, screening tools, withdrawal syndromes, and evidence-based management strategies.
Definition
- Alcohol use refers to the consumption of ethanol-containing beverages.
- Alcohol dependence is characterised by tolerance, withdrawal, and loss of control over use.
Why Do People Drink?
- Pleasure (taste, relaxation)
- Anxiolytic effects (reduces anxiety)
- Self-medication for trauma, stress, or domestic problems
- Psychiatric comorbidities (e.g. depression, eating disorders, history of abuse)
- Genetic predisposition or family history of alcoholism
Mechanism of Action
- ↑ GABA activity → CNS inhibition
- ↓ Glutamate activity → ↓ excitatory tone
- Stimulates mesolimbic dopamine reward pathway
Epidemiology
- Alcohol contributes to:
- 50% of assaults
- 30% of road traffic accidents
- 12% of suicides
- 10% of industrial injuries
- Male consumption patterns:
- 48% drink weekly
- 12% drink daily
- 10% drink at hazardous levels
- Female consumption patterns:
- 35% drink weekly
- 6% drink daily
- 10% drink at hazardous levels
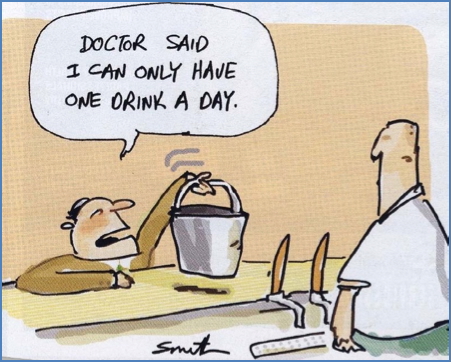
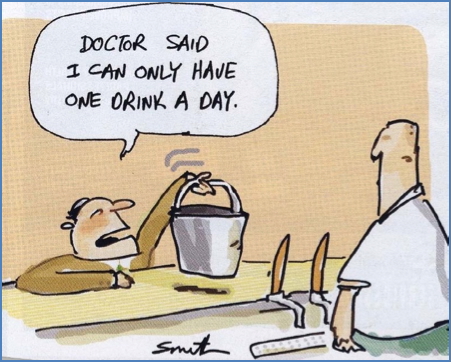
Alcohol Measurement
- 1 standard drink = 10g pure alcohol
- = 30ml spirits
- = 285ml beer
- = 100ml wine
- = 60ml port
- Alcohol content can be calculated using:
- Volume × %Alcohol × Specific Gravity (0.789) ÷ 10 = standard drinks
Clinical Features
Adverse Effects
Psychosocial:
- Relationship breakdown
- Domestic violence
- Crime and driving offences
- Depression, anxiety, irritability, memory loss
- Suicide attempts
Physical:
- Brain damage (irreversible)
- Wernicke-Korsakoff syndrome
- Epilepsy
- Liver disease (fatty liver, hepatitis, cirrhosis)
- Cardiovascular: hypertension, cardiomyopathy
- Gastrointestinal: ulcers, gastritis, pancreatitis
- Endocrine/metabolic: obesity, osteoporosis, gynecomastia, gout
- Haematological: macrocytic anaemia, thrombocytopenia, leukopenia
- Cancer (liver, gastrointestinal tract, head and neck)
- Neurological: tremors, peripheral neuropathy (e.g. Dupuytren’s contracture)
Alcohol Dependence
- Defined by tolerance, compulsive use, and withdrawal symptoms
- Early-onset drinking (<15 years) increases risk of dependence 4-fold
Screening Tools
- CAGE Questionnaire (score ≥2 suggests dependence):
- Cut down
- Annoyed
- Guilty
- Eye-opener
- AUDIT (Alcohol Use Disorders Identification Test)
- 10 questions, risk-tiered score
- Gender-adjusted thresholds


Biological Markers
- ↑ Mean corpuscular volume (MCV)
- ↑ Gamma-glutamyl transferase (GGT)
- Fatty liver
- Hepatitis
- Cirrhosis
Alcohol Withdrawal
- One of the only two life-threatening withdrawal syndromes (other: benzodiazepines)
- Mortality: 2–10% (commonly from arrhythmia or pneumonia)
- Severity assessed via CIWA score
Symptoms
Simple withdrawal:
- Anxiety, agitation, insomnia, depression
- Tremor
- Nausea, vomiting
- Sympathetic overdrive: tachycardia, sweating
Complex withdrawal – Delirium Tremens:
- Onset: 1–14 days post-cessation
- Lasts: 1–6 days
- Predisposing factors:
- Age >30
- Daily heavy use
- Prior DTs or withdrawal seizures
- ↑GGT or MCV
- Concurrent alcohol-related disease
DT Pathophysiology:
- ↑ Cardiac workload
- Hyperventilation → respiratory alkalosis → ↓ cerebral perfusion
- Electrolyte disturbances:
- ↓ potassium (renal losses)
- ↓ magnesium (→ seizures)
- ↓ phosphate (→ heart failure)
Clinical features:
- Tonic-clonic seizures
- Hypervigilance, hallucinations, agitation
- Hyperthermia, hypertension
- Arrhythmias, cardiac arrest
- Risk of stroke
Management
Withdrawal Treatment
- First-line: diazepam (benzodiazepine taper)
- Supportive care:
- Antiemetics, antidiarrhoeals
- Electrolyte repletion
- Vitamin B1 (thiamine) supplementation
Preventative Measures
- Early recognition and brief interventions
- Motivational interviewing
- Alcohol history, social/lifestyle assessment
- Physical exam and blood tests (MCV, LFTs)
Pharmacotherapy for Dependence
- Considered in dependent individuals:
- Naltrexone
- Acamprosate
- Disulfiram (less commonly used)
Behavioural Support
- Counselling and CBT
- Goal setting and coping strategies
- Referral to specialist addiction services
Wernicke-Korsakoff Syndrome
- Preventable, but often irreversible neurological complication
- Caused by thiamine deficiency due to chronic alcohol use
- Alcohol impairs thiamine absorption
- Wernicke’s encephalopathy triad:
- Ophthalmoplegia
- Ataxia
- Confusion
- Korsakoff’s syndrome:
- Anterograde and retrograde amnesia
- Confabulation
- Requires urgent parenteral thiamine
- Poorly treated cases → 75% permanent brain damage
- 20% require lifelong institutional care
Summary – Alcohol
Alcohol is a widely consumed central nervous system depressant that impacts physical, psychological, and social health. From neurochemical changes and dependence to withdrawal syndromes and Wernicke-Korsakoff encephalopathy, understanding the full spectrum of alcohol-related complications is essential for safe and effective clinical practice. For a broader context, see our Psychiatry & Mental Health Overview page.