Table of Contents
Overview – Immunological Tolerance
Immunological tolerance refers to the immune system’s unresponsiveness to specific antigens, particularly self-antigens, thereby preventing harmful autoimmunity. This physiological mechanism distinguishes between self and non-self, ensuring that lymphocytes (T and B cells) are selectively activated or silenced based on the antigen encountered. Tolerance can be central (during lymphocyte development) or peripheral (post-development in the body), and failure of these systems can result in autoimmune disorders or inappropriate immune responses to harmless substances like food or pollen.
Definition
- Immunological tolerance: A state in which the lymphoid tissue does not mount an immune response to a specific antigen
- Tolerated antigens are termed “tolerogens”
Importance
- Prevents immune reactivity to self-antigens (autoimmunity)
- Ensures immune silence towards harmless foreign substances (e.g. food, pollen)
- Facilitates successful organ transplantation and maternal-fetal immune tolerance
Types of Tolerance
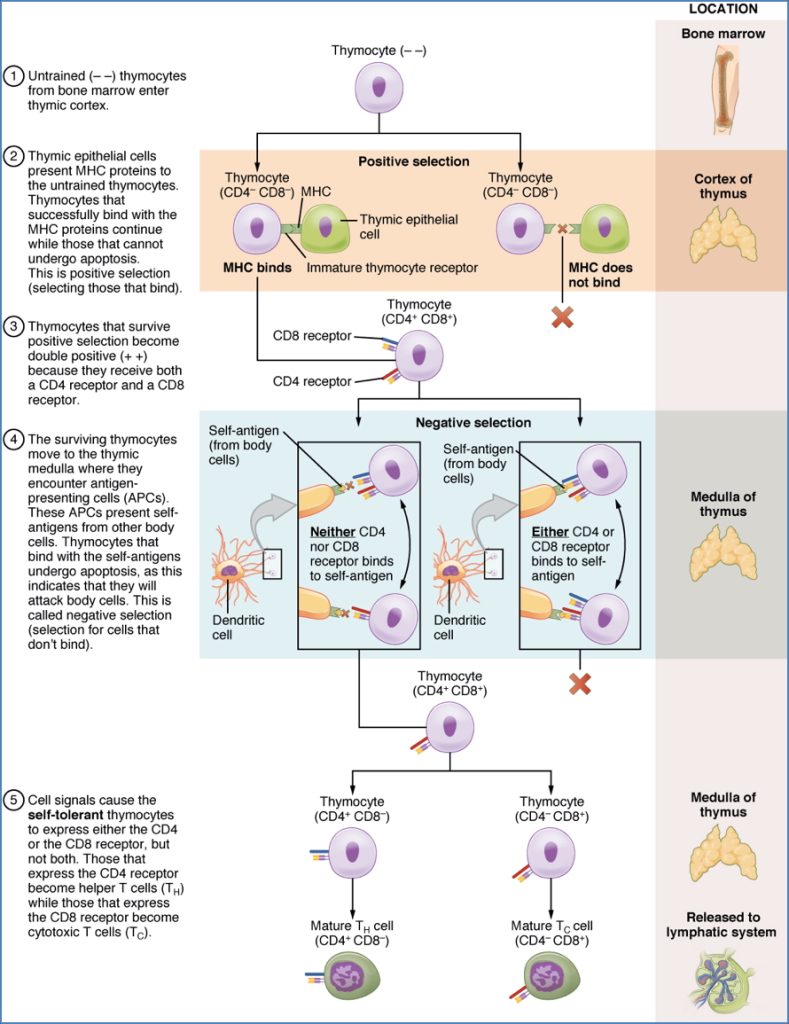
1. Central Tolerance (Self-Tolerance)
Occurs in primary lymphoid organs (bone marrow and thymus) during lymphocyte development.
Mechanism:
- Negative selection of self-reactive T and B cells
- T-cells in thymus
- B-cells in bone marrow
- Clonal deletion: Strongly self-reactive cells undergo apoptosis
- Incomplete exposure to all self-antigens in thymus → necessity for peripheral safeguards
Fail-safes for Escaped Cells:
- B-cells require T-helper cell (Th-cell) support to produce antibodies
- T-cells regulated by peripheral immune mechanisms (see below)
2. Peripheral Tolerance (Acquired Tolerance)
Occurs outside primary lymphoid organs, in secondary lymphoid tissue and the general circulation.
Mechanisms:
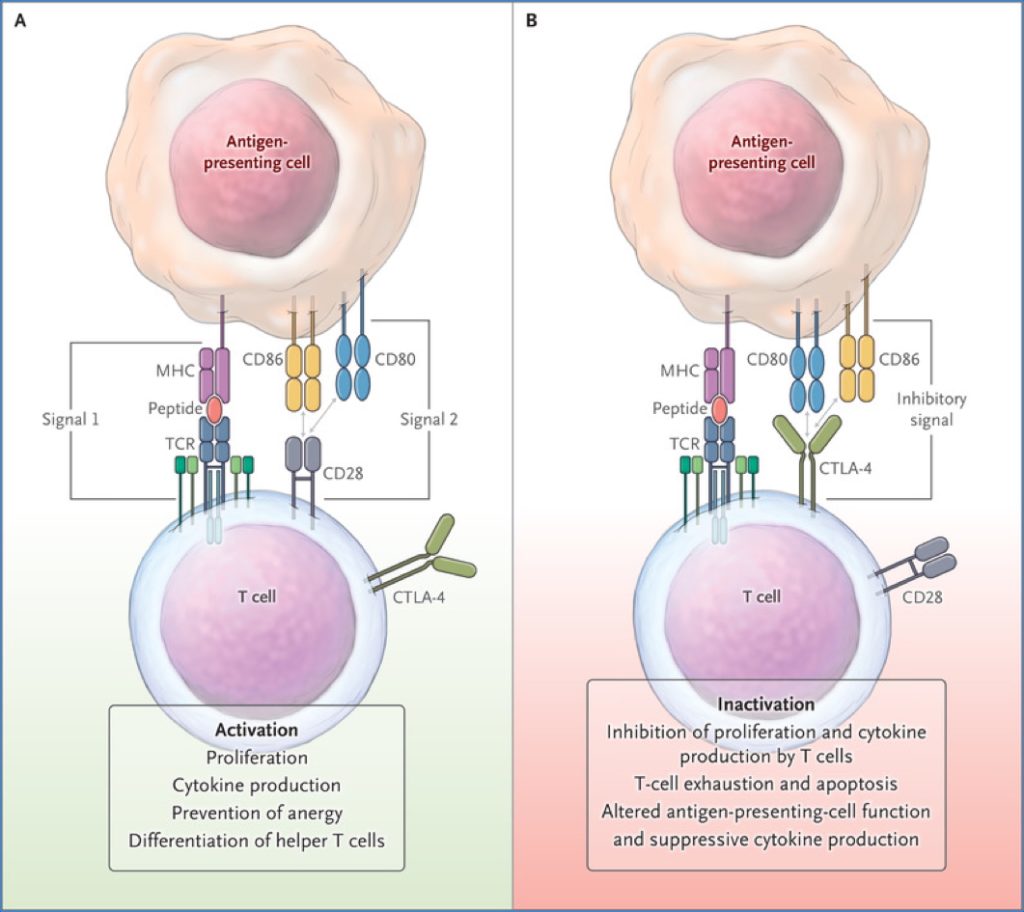
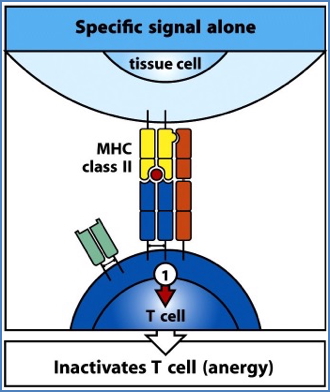
A. Incomplete Activation
- TCR recognition of antigen without co-stimulation or cytokine signalling leads to:
- Anergy (functional inactivation)
- Deletion
- Regulatory T-cell suppression
- Prevents inappropriate activation of escaped auto-reactive T-cells
B. Non-Inflammatory Antigen Exposure
- Exposure to non-pathogenic, non-inflammatory antigens (e.g. dust, food proteins) → immune tolerance
- No cytokine release → APCs fail to express co-stimulatory molecules
- Results in T-cell anergy or suppression
Oral Tolerance
Normal Scenario:
- Food antigens typically induce tolerance, not immunity
- Due to:
- Lack of innate cytokine signalling
- Lack of co-stimulation by APCs
- Inactivation of T-cells when antigen is presented without proper context

Abnormal Scenario (Food Allergy):
- Initial exposure → activation of Th-cells specific to food antigen
- Th-cells activate B-cells → production of food-specific antibodies
- Upon re-exposure:
- Antigen-antibody complexes bind mast cells
- Mast cells degranulate → release histamine
- Results in:
- Vasodilation
- ↑ Vascular permeability
- Cell adhesion molecule upregulation
- Clinical symptoms: cramps, vomiting, diarrhoea, angioedema



3. Oral Tolerance Development and Maintenance; Wambre, Erik et al. Immunology and Allergy Clinics, Volume 38, Issue 1, 27 – 37
Summary – Immunological Tolerance
Immunological tolerance is a critical immune process that prevents self-reactivity and harmful responses to benign antigens, through mechanisms like central deletion and peripheral inactivation of lymphocytes. Oral tolerance further protects against inappropriate immune reactions to dietary antigens. Disruption of these pathways underlies many autoimmune and allergic diseases. For more, see our Immune & Rheumatology Overview page.