Table of Contents
Overview – Control of Breathing
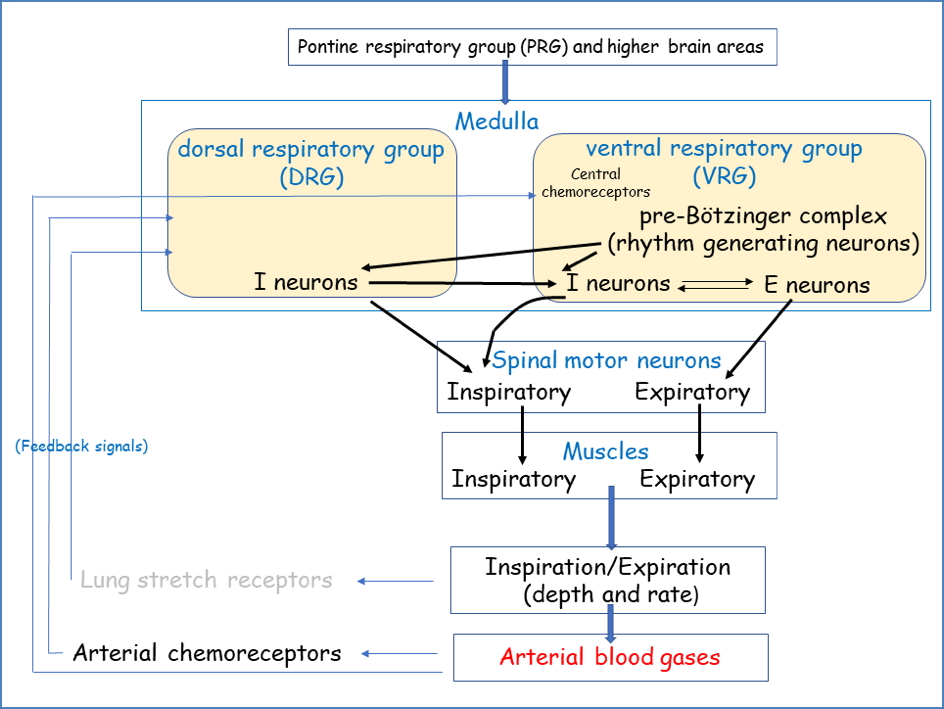
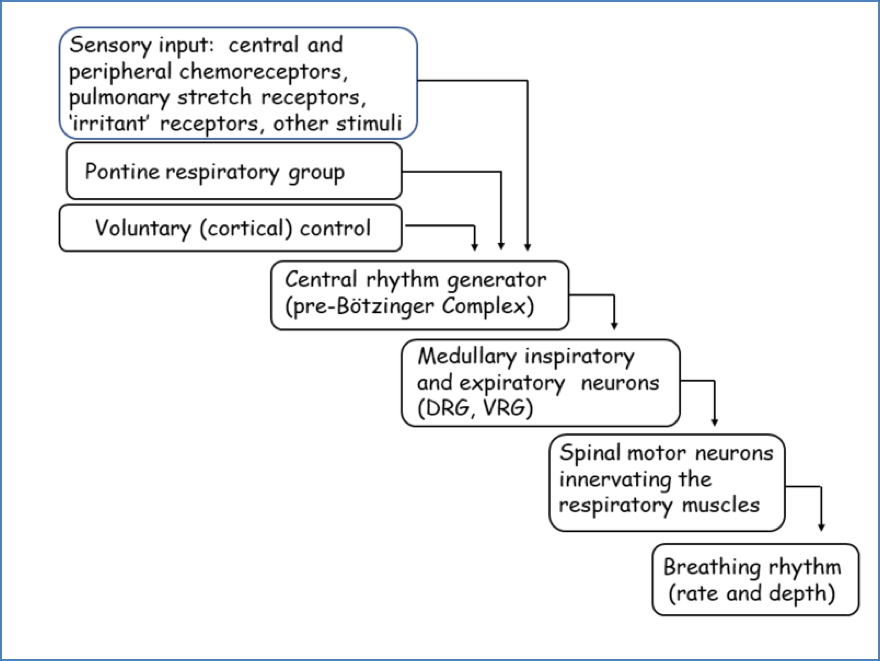
Control of breathing is a vital physiological process that matches alveolar ventilation with metabolic demand. This ensures arterial oxygen (PaO₂) and carbon dioxide (PaCO₂) levels remain stable, even during periods of severe exercise. While venous gas levels may fluctuate significantly, arterial levels are maintained within a narrow range. Breathing is coordinated by the respiratory centres of the medulla and pons, integrating inputs from chemoreceptors, mechanoreceptors, and higher cortical control to generate an uninterrupted rhythm that adjusts automatically to the body’s needs.
Definition
Control of breathing refers to the regulation of respiratory rhythm and depth by central brainstem centres, peripheral receptors, and voluntary cortical pathways, in order to maintain homeostasis of arterial blood gases and acid–base balance.
Central Regulation of Breathing
Overview
- Input from:
- Chemoreceptors (medulla chemosensitive area, aortic bodies, carotid bodies).
- Mechanoreceptors (stretch receptors in lungs).
- Respiratory centre:
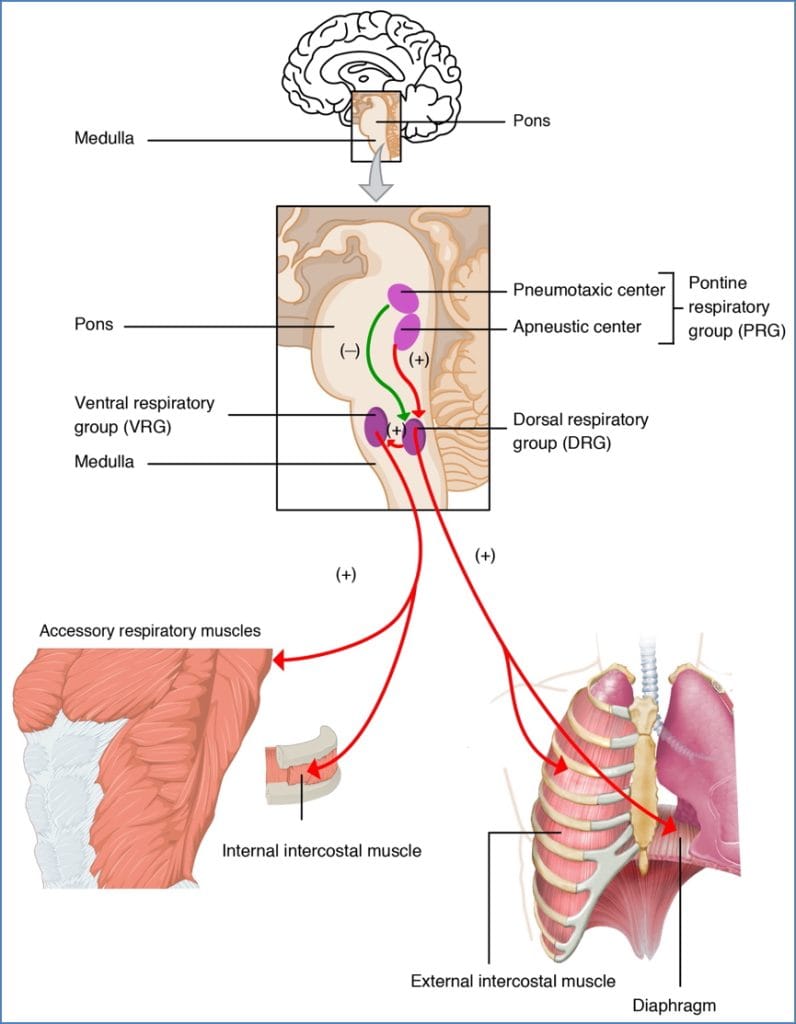
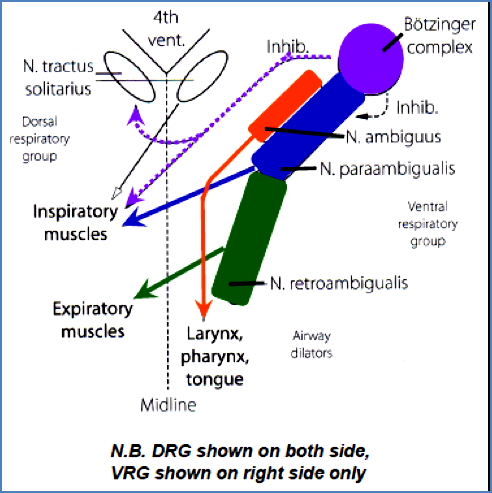
- Medulla: dorsal respiratory group (DRG), ventral respiratory group (VRG).
- Pons: pontine respiratory group (PRG).
- Cerebral cortex: voluntary override.
- Output to:
- Respiratory muscles (diaphragm, intercostals, abdominals).
Medulla (DRG & VRG)
Dorsal Respiratory Group (DRG)
- Location: bilaterally in dorsal medulla, adjacent to the nucleus tractus solitarius.
- Main function:inspiration
- Initiates respiratory rhythm and determines cycle timing.
- Operates via inspiratory ramp signals:
- Signal starts weak and steadily increases over ~2 sec.
- Ceases for ~3 sec, allowing passive exhalation by elastic recoil.
- Can be modified to adjust breathing:
- ↑ speed = steeper ramp signal.
- ↑ rate = early termination of ramp (pneumotaxic influence).
- Inputs: peripheral chemo-, baro-, and mechanoreceptors via glossopharyngeal (CN IX) and vagus (CN X) nerves.
- Outputs:
- Phrenic nerve (C3–C5) → diaphragm.
- Intercostal nerves (T1–T11) → intercostal muscles.


Ventral Respiratory Group (VRG)
- Location: lateral medulla, beside DRG.
- Main function:forced expiration
- Important for active expiration (abdominal muscles, internal/innermost intercostals).
- Inactive during quiet breathing.
- Not rhythm-generating, but recruited under ↑ demand.
- Subdivisions:
- Botzinger complex – inspiratory and expiratory roles (largely unknown).
- Nucleus ambiguus – maintains airway patency (dilator function of larynx, pharynx, tongue).
- Nucleus para-ambigualis – inspiratory muscle activation on opposite body side.
- Nucleus retro-ambigualis – expiratory muscle activation on opposite body side.
Pons – Pontine Respiratory Group (PRG)
- Pneumotaxic centre (upper pons):
- Off-switch for DRG ramp signal.
- Limits inspiration, increases frequency, reduces tidal volume.
- Apneustic centre (lower pons):
- Prolongs ramp signal.
- Lengthens inspiration, reduces frequency, increases tidal volume.
Cerebral Cortex
- Provides conscious override of automatic breathing.
- Acts directly on respiratory muscles, bypassing brainstem centres.
- Important for: speech, singing, sniffing, coughing, playing wind instruments.
Peripheral Input
Upper Respiratory Reflexes
- Cough and sneeze reflexes.
- Receptors in nose, pharynx, larynx.
- Respond to toxins, irritants, and temperature.
Lung Reflexes
- Slowly adapting stretch receptors (SARs):
- Located in airways.
- Detect lung inflation/deflation (volume sensors).
- Rapidly adapting stretch receptors (RARs):
- Detect tidal volume, compliance, and frequency changes.
- Also nociceptive and chemosensitive.
- Inflation reflex (Hering–Breuer):
- Prevents over-inflation by terminating inspiratory ramp via vagus → DRG.
- Deflation reflex:
- Prevents collapse by stimulating inspiration when lung volume is too low.
Chemical Control
- ↑ Arterial CO₂:
- Central chemoreceptors (medulla):
- CO₂ diffuses into CSF → forms H⁺ via bicarbonate buffer.
- H⁺ cannot cross BBB, so CO₂ is the indirect driver.
- Potent, but indirect stimulus of respiratory centre.
- Peripheral chemoreceptors (carotid/aortic bodies):
- Respond to ↑ arterial H⁺ from CO₂ hydration.
- ↑ H⁺ → stimulates ventilation; ↓ H⁺ → depresses ventilation.
- Central chemoreceptors (medulla):

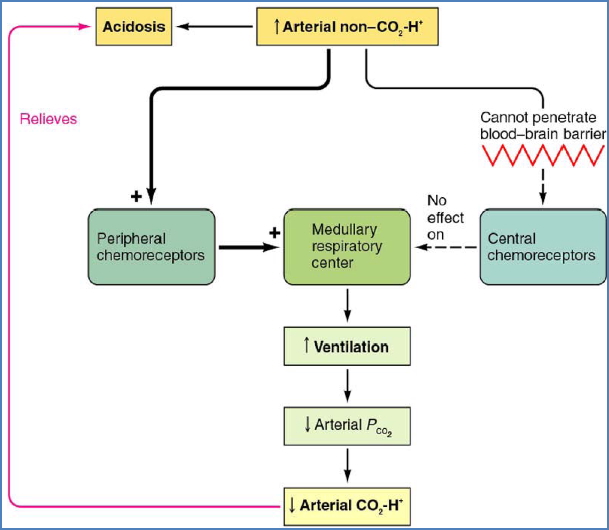
- Non-CO₂ H⁺:
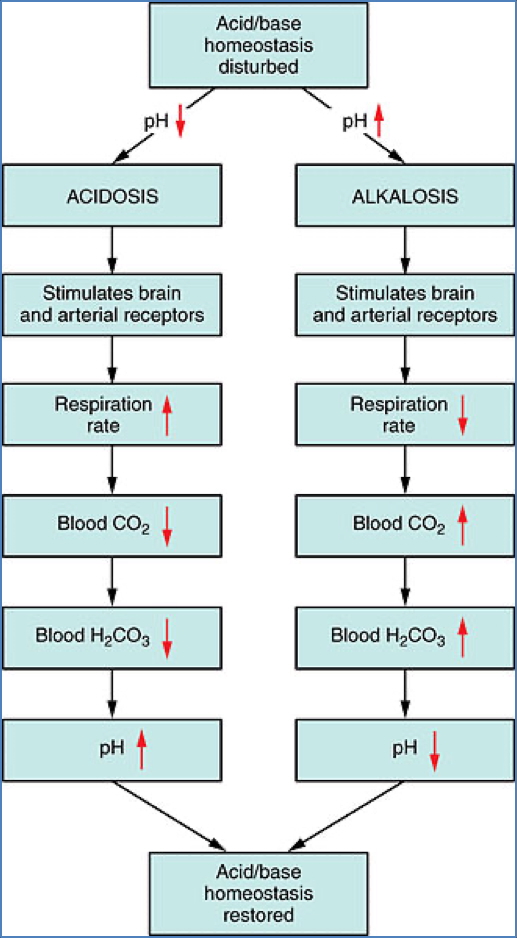
- Peripheral chemoreceptors detect acidosis from lactic acid, ketoacids, etc.
- Drives respiratory compensation for metabolic acidosis/alkalosis.
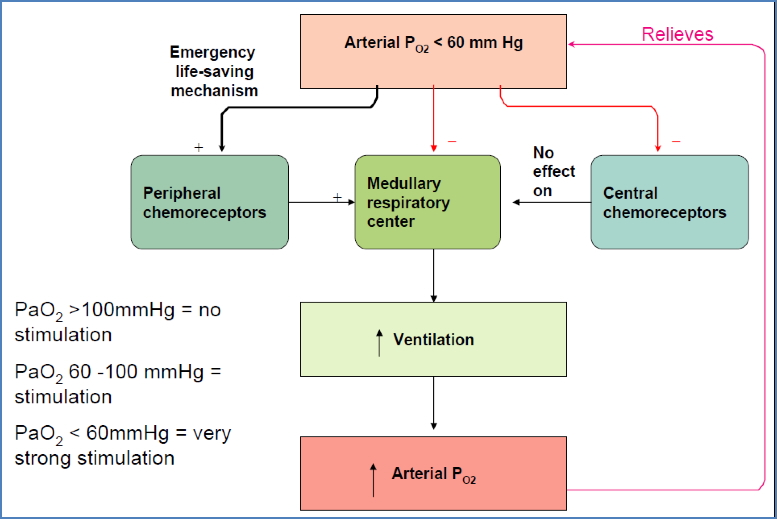
- ↓ Arterial O₂:
- Carotid/aortic bodies strongly stimulate respiration if PaO₂ < ~100 mmHg.
- High perfusion ensures arterial blood is sampled accurately.
- Acclimatisation: in chronic hypoxia (e.g. high altitude), central CO₂ sensitivity decreases, and hypoxia becomes the main respiratory drive.


Mechanical Stimulation
- Baroreceptors:
- ↓ BP → ↑ respiratory rate.
- ↑ BP → ↓ respiratory rate.
- J-receptors:
- Located in alveolar walls, near pulmonary capillaries.
- Stimulated during oedema or engorgement.
- Function still unclear.
Ventilatory Response to Exercise
- Gas levels remain stable; ventilation tightly matches demand.
- Light–moderate: ventilation rises linearly with O₂ consumption.
- Severe: O₂ consumption exceeds supply → anaerobic metabolism.
- Lactic acid accumulation → metabolic acidosis → hyperventilation.


Disorders of Respiratory Regulation
- Ondine’s Curse (Primary Alveolar Hypoventilation Syndrome):
- Loss of automatic respiratory drive.
- Patients must consciously remember to breathe.
- Require ventilatory support during sleep.
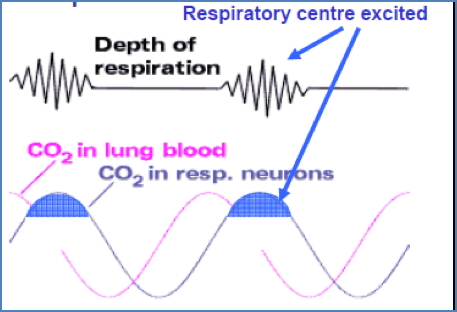
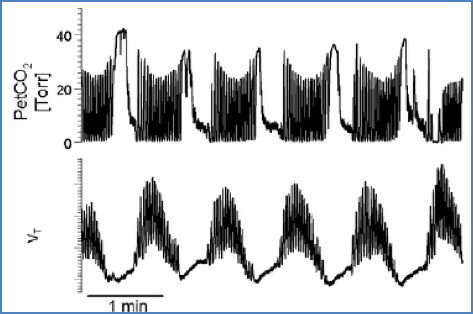
- Cheyne–Stokes Respiration:
- Cyclic pattern of overbreathing and underbreathing.
- Mechanism:
- Overbreathing → ↓ CO₂, ↑ O₂.
- Circulation delay delays brain feedback.
- Respiratory centre suppressed excessively.
- Underbreathing follows → ↑ CO₂, ↓ O₂.
- Delayed feedback causes overshoot of ventilation.
- Causes: cardiac failure, CNS injury, prolonged circulation time, heightened negative feedback gain.
- Sleep Apnoea:
- Obstructive: intermittent airflow blockage despite ongoing effort.
- Central: cessation of effort due to absent drive from DRG.
Summary – Control of Breathing
Control of breathing is coordinated by medullary and pontine centres, influenced by chemoreceptors, mechanoreceptors, and cortical override. These systems ensure arterial gas stability across rest, exercise, and metabolic challenges, while reflexes protect against overinflation or collapse. Clinical conditions such as Ondine’s curse, Cheyne–Stokes respiration, and sleep apnoea highlight the vital importance of this regulation. For further context, see our Respiratory Overview page.