Table of Contents
Overview – Raised Intracranial Pressure
Raised intracranial pressure (ICP) occurs when the pressure inside the skull exceeds normal levels, threatening cerebral perfusion and risking brain herniation. It can result from trauma, tumours, haemorrhage, hydrocephalus, or cerebral oedema. Recognising Cushing’s reflex, avoiding lumbar puncture, and understanding emergency interventions like mannitol and CSF shunts are vital in acute neurocritical care.
Normal Physiology
- Normal ICP: ~10 mmHg
- Cerebral Perfusion Pressure (CPP) = Mean Arterial Pressure – ICP
- If ICP rises to match arterial pressure → CPP = 0 → No cerebral perfusion → Brain ischaemia
Clinical Signs of Raised ICP
Cushing’s Triad (Late Sign)
- Hypertension
- Bradycardia
- Irregular or Cheyne-Stokes breathing
Other Symptoms
- Headache
- Vomiting
- Altered level of consciousness
- Pupillary abnormalities (e.g. CN III palsy)
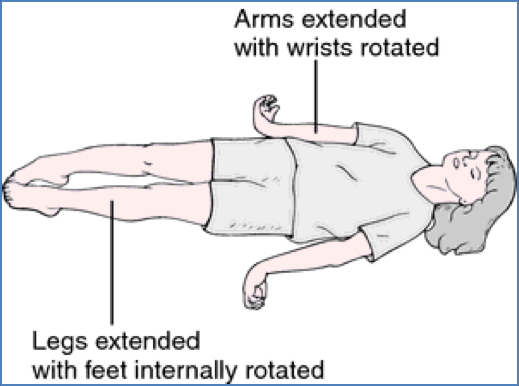
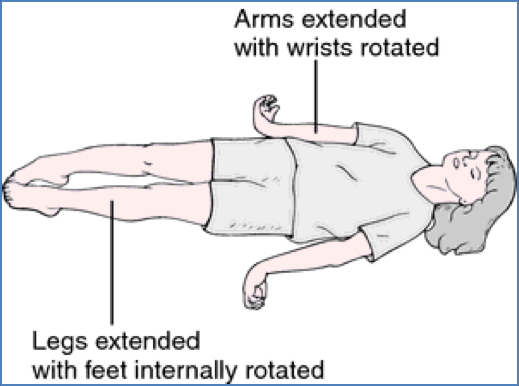
- Decerebrate posturing (late/terminal)
Cerebral Oedema
Definition
- Accumulation of fluid within brain tissue → ↑ICP
Types of Cerebral Oedema
| Type | Mechanism | Examples |
|---|---|---|
| Vasogenic | ↑Capillary permeability | Trauma, infection, infarction |
| Cytotoxic | Cell swelling from Na⁺/H₂O retention | Hypoxia, neurotoxins |
| Osmotic | Plasma < CSF osmolality | Water intoxication, hyponatraemia |
| Interstitial | CSF transudation into brain | Obstructive hydrocephalus |
Shared Clinical Features
- Features of underlying cause
- Signs of ↑ICP: headache, vomiting, ALOC, blown pupils, Cushing’s triad
Management of Raised ICP
| Treatment | Mechanism |
|---|---|
| Osmotic Diuretics (Mannitol) | Draws fluid out of brain → ↓ICP |
| Hyperventilation | ↓PaCO₂ → cerebral vasoconstriction → ↓CBF and ICP |
| CSF Drainage / Shunt | Directly removes CSF volume |
| Surgical Intervention | For haemorrhage, mass lesion, or hydrocephalus |
| Head elevation (30–40°) | Aids venous drainage |


Critical Warning
Do NOT perform a lumbar puncture in suspected raised ICP.
Why?
- Sudden removal of CSF can trigger brain herniation (coning)
- Herniation through foramen magnum → medullary compression → coma or death
Herniation Signs
- GCS 3–5
- Vomiting
- Unilateral dilated pupil (CN III palsy)
- Abnormal posturing
Brain Herniation Syndromes
| Type | Pathogenesis | Clinical Features |
|---|---|---|
| Cerebellar Tonsillar (Coning) | Cerebellar tonsils herniate through foramen magnum → brainstem compression | ALOC, decerebrate posturing, vomiting, CN III palsy, respiratory arrest |
| Uncal Herniation | Uncus of temporal lobe herniates over tentorium → midbrain compression | Ipsilateral CN III palsy (ptosis, dilated pupil, down/out gaze), hemiparesis |
| Subfalcine Herniation | Cingulate gyrus herniates under falx cerebri | May compress ACA → contralateral leg weakness, abulia |


Summary – Raised Intracranial Pressure
Raised intracranial pressure is a life-threatening complication of brain injury, infection, haemorrhage, or tumour. Classic signs include Cushing’s triad, vomiting, altered consciousness, and cranial nerve palsies. Management includes mannitol, hyperventilation, and surgical drainage—but avoid lumbar puncture when ICP is high to prevent fatal brain herniation. For a broader context, see our Nervous System Overview page.