Table of Contents
Overview – The Musculoskeletal Examination
The musculoskeletal (MSK) examination involves a structured assessment of bones, joints, ligaments, muscles, and related neurological function. It is essential in evaluating joint pain, stiffness, trauma, and systemic diseases like rheumatoid arthritis and polymyalgia rheumatica. Core components include history-taking, screening exams like GALS, and focused joint assessments including special tests for pathology.
Musculoskeletal History
- Presenting Complaint: Pain, stiffness, trauma, movement limitation
- History of Presenting Complaint:
- Acute vs Chronic
- Mechanism of Injury – Critical to identify!
- Symptoms:
- Pain vs tenderness (consider referred pain) → Use NILDOCARF
- Movement limitation:
- Pain-related: Tendinopathy, impingement, sprain, labral tear
- Mechanical block: Labral, frozen shoulder
- Instability (clicking/clunking)
- Joint swelling
- Night pain: Consider rotator cuff, AC joint injury, collateral knee ligaments, bone cancer
- Rheumatological Associations: Fever, weakness, fatigue, weight loss, iritis
- Progression: Better, worse, or static
- Past Medical, Drug, Family, Social History
- Red Flags (urgent and dangerous):
- Open fractures
- Neurovascular compromise
- Cauda equina syndrome
- Bone/joint infections
- Acute compartment syndrome
- Cancer
- Temporal arteritis (especially in PMR patients)
- Cardiac mimic (e.g., MI presenting as chest wall pain)
- Yellow Flags: Psychosocial factors mimicking MSK pathology (e.g., depression with back pain)
GALS Screen (Gait, Arms, Legs, Spine)
Introduction
- Wash hands, obtain consent
- Ensure adequate exposure (remove shirt, pants, shoes)
Gait
- Observe while patient walks across the room and back:
- Fluidity, symmetry, antalgic gait, foot drop (L4/L5)
Arms
- Shoulder & Elbow:
- Raise hands overhead, then behind head and push back
- Touch fingers to shoulders and raise elbows
- Lock elbows to side → external rotation
- Thumb up spine → internal rotation
- Push arms behind back → extension
- Cross-body reach → adduction
- Supination and pronation
- Hands & Fingers:
- Finger splay + resisted compression
- Fingers together + resisted separation
- Grip strength
- Make a fist
- Touch thumb to each fingertip
- MCP squeeze test for tenderness
Legs
- Functional Testing:
- 3x half squats (patellofemoral joint)
- 1x full squat (knee joint proper)
- Ankle inversion, eversion
- Dorsiflexion, plantarflexion
- Toe splay and scrunch
Spine
- Observe: Kyphosis, lordosis, scoliosis
- Lumbar flexion: Touch toes
- Lumbar extension: Look at ceiling
- Lateral flexion: Slide hand down leg
- Neck: Flexion (chin to chest), extension (look up), lateral flexion, and rotation
Reporting Format
- G – Gait: Normal/Abnormal + Comments
- A – Arms: Normal/Abnormal + Comments
- L – Legs: Normal/Abnormal + Comments
- S – Spine: Normal/Abnormal + Comments e.g. “Abnormal Arm: Limited abduction of shoulder to 90°”
Focused Joint Examination Algorithm (Shoulder or Knee)
Look
- Compare both sides for:
- Symmetry
- Scars
- Redness, bruising
- Swelling, lumps
- Muscle wasting
Feel
- Palpate relevant structures for:
- Tenderness (objective)
- Warmth, swelling, crepitus (subjective)
- Warmth → Inflammation, trauma, infection
- Crepitus → OA, tendinopathy
- Swelling → Effusion or soft tissue mass
Move
- Active Movement in all planes
- Observe symmetry, range of motion (ROM), pain, fluidity
- If limited → Ask: “Why?” → Blockage, weakness, or neurological
- Passive movement only if active movement limited
Measure
- Compare ROM with opposite side (ballpark, not formal goniometry) e.g. “Limited active extension of left elbow to 150°”
Special Tests (Based on Clinical Context)
Shoulder
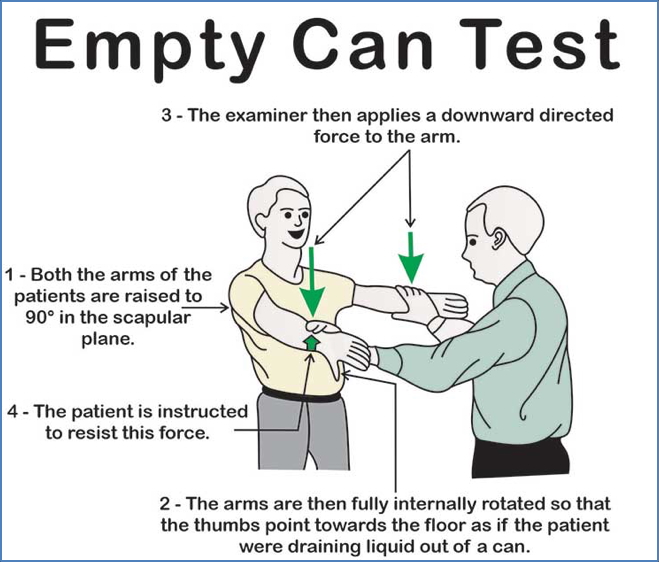
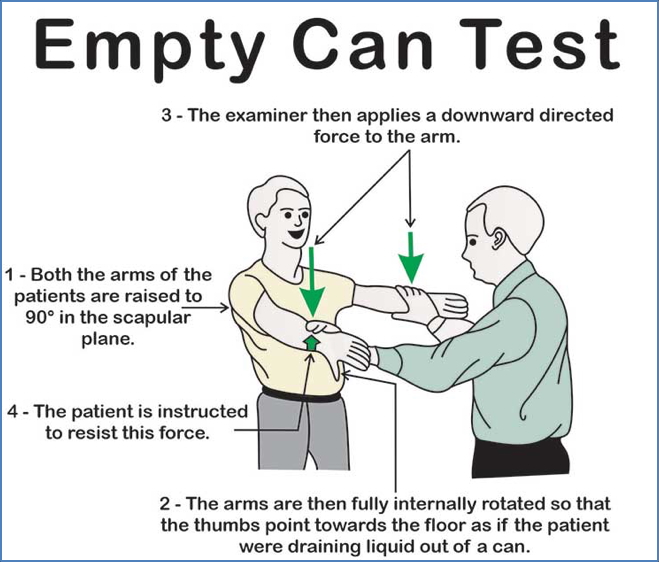
- Supraspinatus tear:
- Empty Can Test
- Drop Arm Test
- Impingement (subacromial):
- Instability:
- Apprehension & Relocation Test








Knee
- ACL tear:
- Lachman’s Test
- Anterior Drawer Test (less useful if awake)


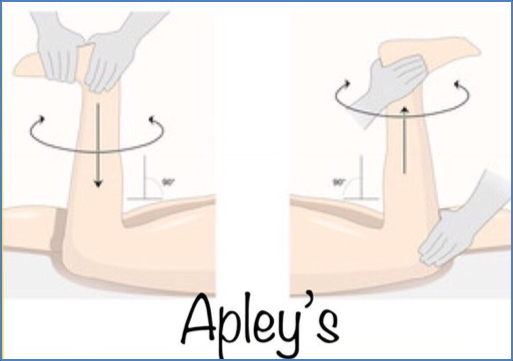
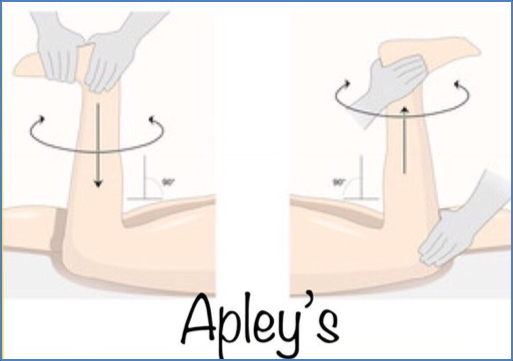
- Meniscal tear:
- Thessaly Test
- Apley’s Grind Test


2. https://twitter.com/peds_sports_med/status/1041163674436730881?lang=ca
- Collateral ligament tear:
- Varus/Valgus Stress Test


- Patellofemoral syndrome:
- Half squats → Elicits anterior knee pain
Focused Shoulder Examination
Look
- Compare symmetry, scars, bruising, swelling, atrophy
Feel
- Palpate both shoulders (bilateral)
- Structures:
- Sternoclavicular joint
- Clavicle
- AC joint
- Glenohumeral joint
- Spine of scapula, scapular borders
- Assess for: Tenderness, warmth, swelling, crepitus
Move & Measure
- Active ROM first → Fluidity, pain, range
- Passive ROM if restricted
- Record measurements “Symmetrical full ROM in all planes” or
“Limited active extension to 150° on left”
Relevant Special Tests
- Tear (Supraspinatus) → Drop Arm Test, Empty Can
- Impingement → Hawkins Test
- Instability → Apprehension & Relocation Test
Focused Knee Examination
Look
- Symmetry, scars, bruising, swelling, atrophy
Feel
- Palpate both knees
- Structures:
- Quadriceps tendon
- Patella + Patellar tap
- Patellar tendon
- Tibial tuberosity
- Joint lines
- Collateral ligament insertions
Move & Measure
- 3x half squats → Patellofemoral
- 1x full squat → Knee joint proper
- Assess: Pain, range, symmetry
- Measure ROM and compare bilaterally
Special Tests
- ACL Tear → Lachman’s, Anterior Drawer
- Meniscal Tear → Thessaly, Apley’s Grind
- Collateral Ligaments → Valgus/Varus stress
- PF Maltracking → Pain on squatting
Summary – The Musculoskeletal Examination
The musculoskeletal examination is an essential clinical skill for identifying joint pathology, injury patterns, systemic disease, and functional limitation. Final-year medical students must master both the GALS screening and focused joint assessments for knees and shoulders, while maintaining a high index of suspicion for serious pathology. For a broader context, see our Clinical Skills Overview page.