Table of Contents
Overview – Infective Endocarditis
Infective endocarditis is a serious and potentially life-threatening infection of the endocardial surface of the heart, most commonly involving the heart valves. It is often associated with underlying structural heart disease, prosthetic valves, or intravenous access. Clinical suspicion must be high in any patient presenting with fever and a new murmur. Early recognition and aggressive treatment are crucial to reduce complications such as embolic events, renal failure, or cardiac damage.
Definition
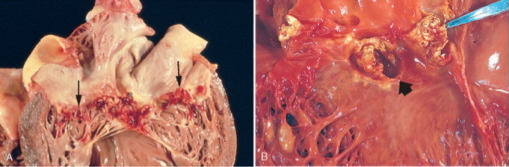
Infective endocarditis is the microbial infection of the endothelial lining of the heart, typically affecting the valves, and characterised by the formation of vegetations composed of bacteria, fibrin, and inflammatory cells.
Risk Factors
- Pre-existing valvular abnormalities (e.g. congenital defects, murmurs, calcific disease)
- Prosthetic heart valves
- Recent open-heart surgery
- Poor dental hygiene or recent dental procedures
- Presence of indwelling IV lines (e.g. haemodialysis catheters)
- Intravenous drug use (IVDU)
- Immunosuppression
Aetiology
Subacute Bacterial Endocarditis (SBE) – 50–60% of cases
- Low virulence organisms
- Streptococcus viridans (oral flora)
- Staphylococcus epidermidis (prosthetic valves)
- Often follows dental procedures or prosthetic valve surgery
Acute Bacterial Endocarditis (ABE) – 10–20% of cases
- High virulence organisms
- Staphylococcus aureus (including MRSA)
- Common in IV drug users
- Rapid onset, high mortality (~50% if untreated)
Pathophysiology
- Bacteria enter the bloodstream and adhere to damaged or prosthetic valves
- Vegetations form on valve cusps (mainly mitral and aortic valves)
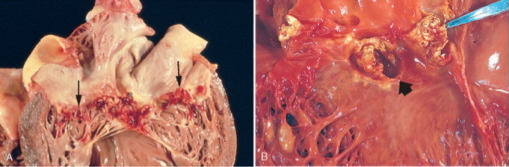
- In IVDU, the tricuspid valve may be involved
- Vegetations can embolise, causing systemic or pulmonary infarcts
Clinical Features
Symptoms
- Fever + New Heart Murmur = endocarditis until proven otherwise
- Constitutional symptoms: fatigue, malaise, anorexia, weight loss
Peripheral Signs of Septic Emboli
- Splinter haemorrhages – linear lesions under fingernails
- Osler’s nodes – painful nodules on finger/toe pads
- Janeway lesions – non-tender macules on palms/soles
- Roth spots – retinal haemorrhages with pale centres
- Splenomegaly, arrhythmias
Complications (typically after 2 weeks)
- Glomerulonephritis – due to immune complex deposition
- Renal failure, haematuria
- Transient Ischaemic Attack (TIA)/Stroke – septic cerebral emboli
- Septicaemia
- Congestive cardiac failure (CCF) – if valvular destruction is significant
Investigations
- Clinical diagnosis: fever + new systolic murmur ± embolic signs
- Blood cultures ×3 (different times/sites to avoid contamination)
- Echocardiogram (TTE or TOE) – detects vegetations, valvular regurgitation
- ECG – rule out ischaemia or arrhythmias
Management
- Empirical IV antibiotics:
- Start with high-dose vancomycin, then tailor based on cultures
- Duration: 2–6 weeks depending on organism and valve type
- Cardiothoracic surgery referral if:
- Valve destruction or severe regurgitation
- Heart failure
- Antibiotic failure
Prognosis
- Treated infective endocarditis has a 30% mortality rate
- Poor prognosis associated with S. aureus, prosthetic valves, and delayed treatment
Summary – Infective Endocarditis
Infective endocarditis is a life-threatening infection of the heart’s endocardial lining, commonly affecting the valves. It presents with fever and a new murmur, and may lead to embolic or renal complications. Diagnosis is clinical, supported by blood cultures and echocardiography. Management includes prolonged IV antibiotics and sometimes surgical valve repair. For a broader context, see our Cardiovascular Overview page.