Table of Contents
Overview – Cardiodynamics
Cardiodynamics refers to the physiological mechanisms that regulate cardiac output by modulating heart rate and stroke volume. These parameters adjust to meet the body’s metabolic demands and ensure effective tissue perfusion. A comprehensive understanding of cardiodynamics is essential for assessing cardiovascular performance in both health and disease, and for interpreting compensatory responses in shock, heart failure, or exercise.
Cardiac Output
- A key measure of cardiac function over time
- Calculated as:
Cardiac Output (mL/min) = Stroke Volume × Heart Rate
- Average CO ≈ 5 L/min — meaning the entire blood volume circulates once per minute
- CO dynamically adjusts to ensure adequate oxygen and nutrient delivery to peripheral tissues
Heart Rate (HR)
Regulation & Terminology
- Reflects beats per minute
- Responds to tissue oxygenation and metabolic demand
- Bradycardia: Slower than normal HR
- Tachycardia: Faster than normal HR
Factors That Affect Heart Rate
1. SA Node Firing
- As the heart’s pacemaker, the SA node sets the rhythm
- Changes in firing rate → change HR → change CO
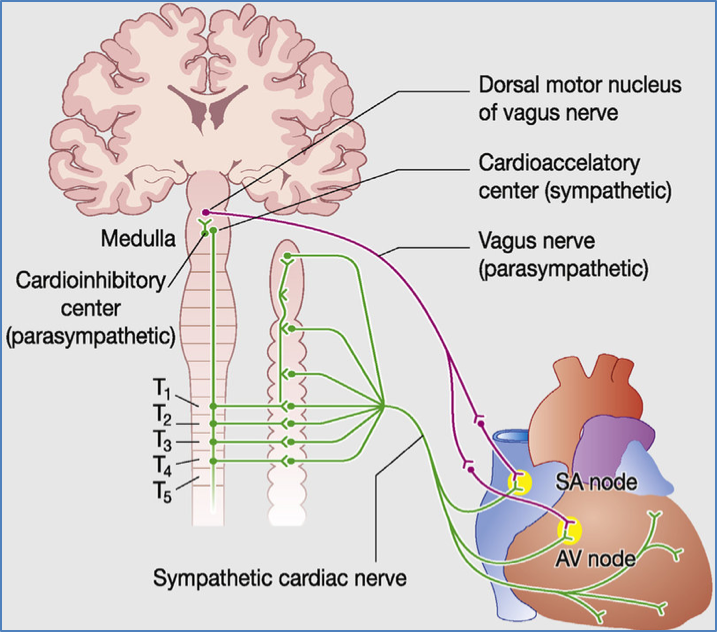
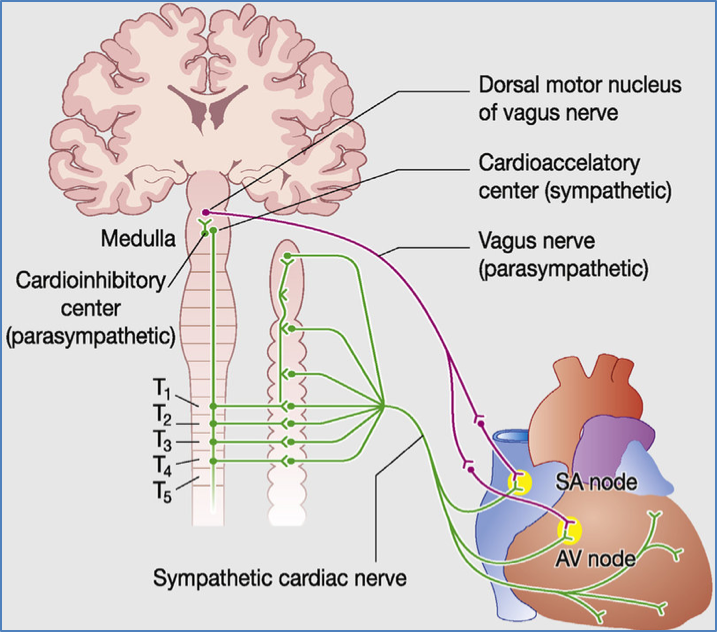
2. Autonomic Nervous System (ANS)
- Parasympathetic (Vagus nerve):
- ↓ HR (−ve chronotropic)
- ↑ AV node delay (−ve dromotropic)
- Minimal effect on contractility
- Sympathetic (Cardiac sympathetic fibres):
- ↑ HR (+ve chronotropic)
- ↑ Contractility (+ve inotropic)
3. Reflex Controls
- Bainbridge Reflex (Atrial Stretch):
- ↑ Venous return → Atrial stretch receptors → ↑ Sympathetic output → ↑ HR
- Accounts for ~40–60% of HR increase
- Chemoreceptor Reflex:
- Low O₂ / High CO₂ → ↑ HR and respiration rate
- Baroreceptor Reflex (Aortic + Carotid):
- ↑ BP → ↑ receptor stretch → ↓ HR and ↓ contractility
- Mediated by:
- Aortic baroreceptors → Vagus nerve
- Carotid baroreceptors → Hering’s nerve
- Receptors adapt in chronic hypertension


4. Atrial Node Stretch
- ↑ Venous return stretches SA node cells
- ↑ Stretch → ↑ firing rate → ↑ HR
- Responsible for ~15% of HR increase
- Influenced by:
- Arterial pressure
- Peripheral compliance
- Local tissue perfusion
5. Chemical Regulation
- Hormonal Influences:
- Adrenaline, Thyroxine, Insulin → increase HR
- Ion Concentrations:
- Na⁺, K⁺, Ca²⁺ imbalances can alter nodal depolarisation and HR
Other Modifying Factors
- Age: Older age → ↓ resting HR
- Gender: Females generally have ↑ resting HR
- Fitness: Well-trained individuals → ↓ resting HR
- Temperature: Elevated body temperature → ↑ HR
Stroke Volume (SV)
- Volume of blood pumped per ventricular contraction
- Useful for assessing efficiency of each cardiac cycle
Stroke Volume = End Diastolic Volume (EDV) − End Systolic Volume (ESV)
Factors That Increase Stroke Volume:
- ↑ Ventricular filling time (↑ diastole duration)
- ↑ Venous return
- ↓ Arterial blood pressure (afterload)
- ↑ Ventricular contractility
Determinants of Stroke Volume
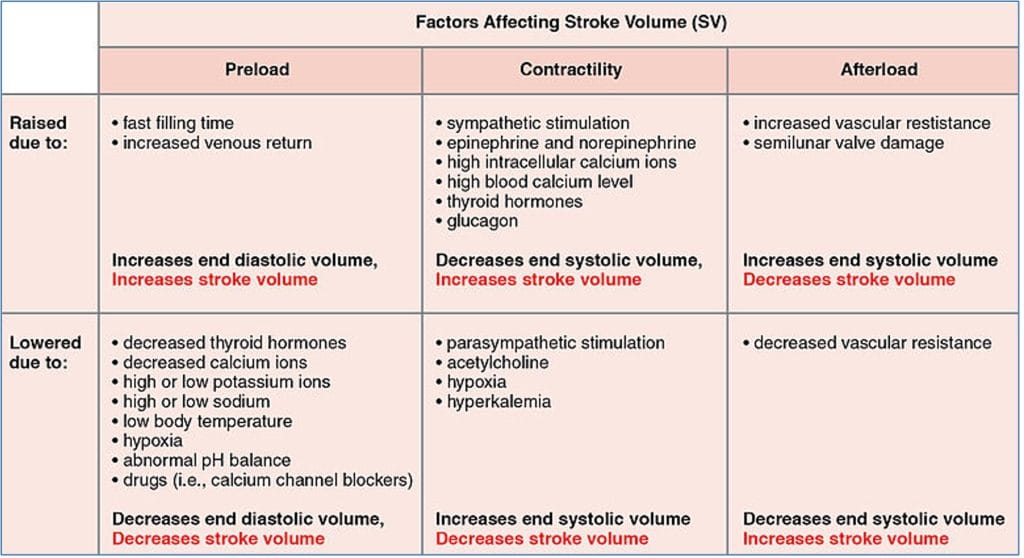
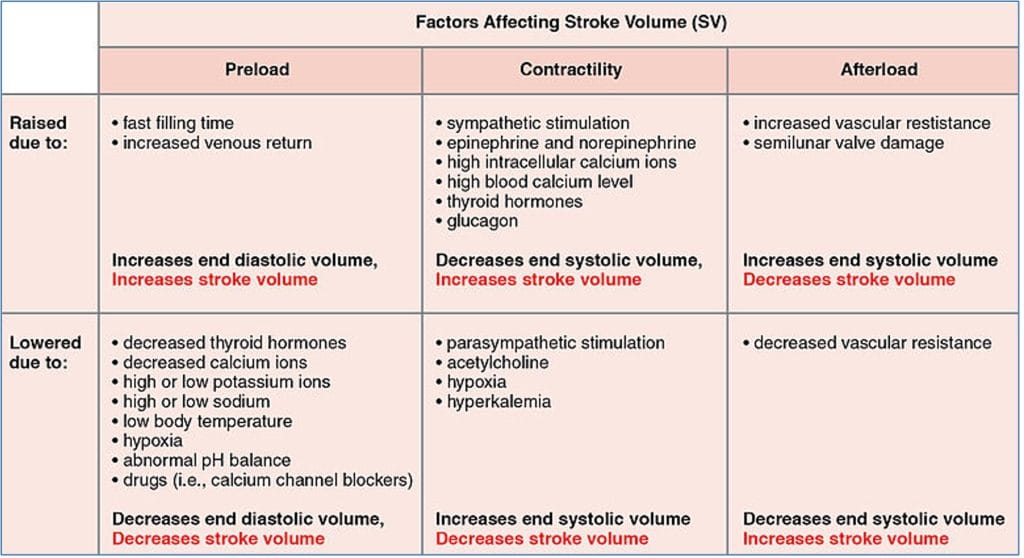
1. Preload
- Stretch of ventricular muscle during diastole
- Proportional to venous return and EDV
- ↑ Preload → ↑ sarcomere length → ↑ contractile strength
- Known as the Frank-Starling mechanism
- Influenced by:
- Arterial pressure
- Capillary exchange
- Local blood flow
- Peripheral compliance
- Contractility (Inotropy):
- Force of contraction at a given preload
- ↑ Contractility → ↓ ESV → ↑ SV
2. Afterload
- The back pressure the ventricle must overcome to open the semilunar valve
- ↑ Afterload → ↑ ESV → ↓ SV
- Increased by:
- Arterial hypertension
- Aortic or pulmonary valve stenosis
- Vascular resistance
Summary – Cardiodynamics
Cardiodynamics describes how stroke volume and heart rate interact to determine cardiac output. These are regulated through neural, reflexive, and chemical mechanisms, as well as by intrinsic myocardial properties like preload, afterload, and contractility. A strong grasp of these principles helps in evaluating cardiovascular performance across a wide range of clinical contexts. For a broader context, see our Cardiovascular Overview page.