Table of Contents
Overview – Urinary Incontinence
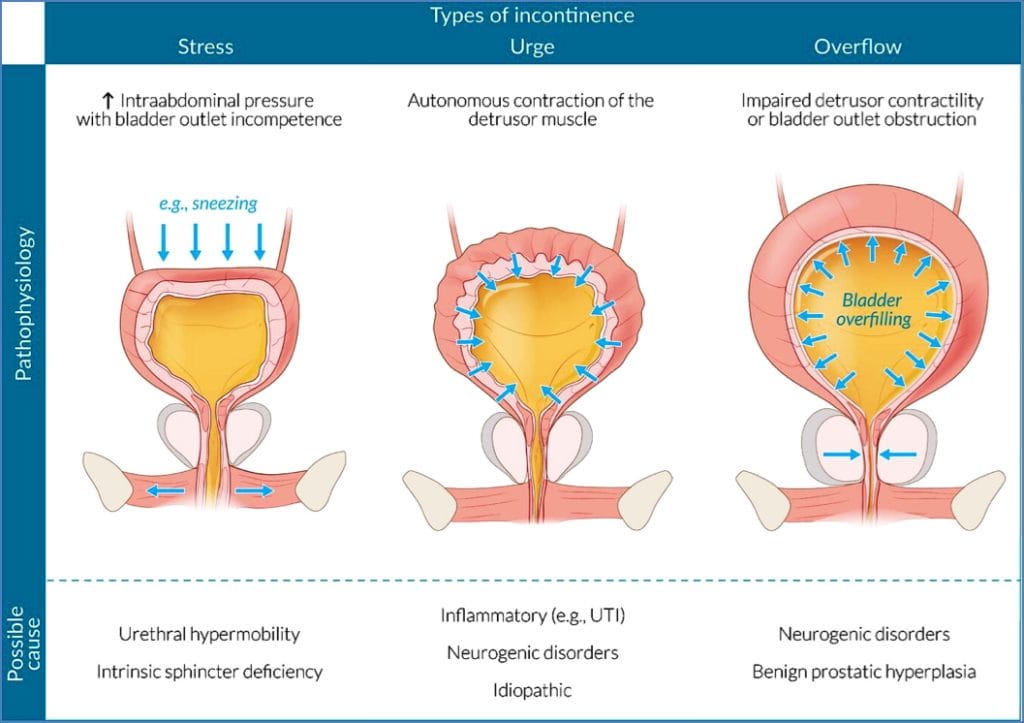
Urinary incontinence refers to the involuntary leakage of urine due to a loss of control over micturition. It is a common clinical issue, particularly in older adults and females, and significantly impacts quality of life. There are several types, each with distinct causes, mechanisms, and management strategies. This article outlines the clinical features, pathophysiology, diagnosis, and treatment of overflow, stress, and urge incontinence.
Definition
- Urinary incontinence is the inability to voluntarily control urine output, resulting in involuntary leakage.
Overflow Incontinence
Aetiology
- Obstructive causes:
- Benign prostatic hyperplasia (BPH)
- Prostate cancer
- Urethral stricture
- Cystocele
- Uterine prolapse
- Neurogenic bladder:
- Diabetic neuropathy
- Spinal cord injury
- Cauda equina syndrome
- Anticholinergic medications
Pathogenesis
- Chronic urinary retention leads to rising bladder pressure
- When pressure exceeds urethral resistance → small, frequent leakages
Clinical Features
- Continuous or frequent dribbling of small amounts of urine
- Hesitancy
- Weak or intermittent stream
Diagnosis
- Urologic history and physical examination
- Abdominal ultrasound
- Urodynamic studies
Treatment
- Cholinergic agents (↑ detrusor tone)
- Alpha-blockers (e.g. prazosin, tamsulosin) → relax bladder outlet
- Intermittent self-catheterisation
- Surgery (if indicated)
Stress Incontinence
Aetiology
- Pelvic floor weakness
- Most common in women under 70
- Risk factors:
Pathogenesis
- Lax pelvic support → urethral hypermobility
- Intra-abdominal pressure (e.g. coughing, sneezing) exceeds sphincter resistance
Clinical Features
- Leakage with exertion, coughing, laughing, or exercise
Diagnosis
- Urologic history
- Abdominal ultrasound
- Urodynamic studies
Treatment
- Pelvic floor (Kegel) exercises
- Hormone replacement therapy (HRT) in postmenopausal women
- Weight loss
- Surgical sling procedures
Urge Incontinence
Aetiology
- Overactive bladder (detrusor instability)
Pathogenesis
- Involuntary bladder contractions cause sudden urge and leakage
Clinical Features
- Sudden, strong urge to void
- Large-volume leakage
- Increased frequency
- Nocturia or nocturnal wetting
Diagnosis
- Urologic history
- Abdominal ultrasound
- Urodynamic testing
Treatment
- Anticholinergic agents (e.g. oxybutynin)
- Tricyclic antidepressants (e.g. amitriptyline)
- Intradetrusor botulinum toxin injections
- Bladder training
- Pelvic floor exercises
- Surgery (e.g. sling procedures, in refractory cases)
Summary – Urinary Incontinence
Urinary incontinence encompasses multiple subtypes including overflow, stress, and urge incontinence—each with specific aetiologies, pathophysiology, and treatments. Accurate diagnosis through urologic history, imaging, and urodynamic studies is essential for targeted therapy. A combination of pharmacological, behavioural, and surgical interventions can significantly improve outcomes. For a broader context, see our Renal Overview page.