Table of Contents
Overview – Traumatic Brain Injuries
Traumatic brain injuries (TBIs) are a leading cause of morbidity and mortality, particularly in trauma and emergency settings. They can be classified into focal and diffuse injuries, each with characteristic pathophysiology and clinical consequences. Understanding the distinctions between concussion, contusion, laceration, and diffuse axonal injury is vital for accurate diagnosis and management in clinical practice. This page provides a high-yield summary of traumatic brain injuries relevant for final-year medical students.
Definition
Traumatic brain injuries are acute injuries to the brain tissue caused by mechanical force, commonly classified into:
- Focal injuries: Confined to one brain region (e.g. concussion, contusion, laceration)
- Diffuse injuries: Widespread neuronal damage (e.g. diffuse axonal injury)
Aetiology
- Blunt trauma: Falls, road traffic accidents, assault
- Penetrating trauma: Gunshot wounds, stabbing injuries
- Acceleration-deceleration: Whiplash, high-speed collisions
Classification of Primary Brain Injuries
Concussion
- Cause: Moderate blunt trauma
- Mechanism: Disruption of metabolic, ionic, and neurotransmitter balance → impaired neurofunction
- Clinical:
- Temporary LOC (seconds–minutes)
- Anterograde & retrograde amnesia
- Headache, dizziness, visual disturbances
- Post-Concussion Syndrome (up to 3 weeks post-injury): memory issues, photophobia, irritability, fatigue
- Investigations:
- Concussion grading (Grade I–III)
- Neurological exam, GCS
- CT if GCS <14
- Management:
- Supportive care (rest, analgesia)
- Avoid repeat injury (risk of Second Impact Syndrome)
- Prognosis:
- Excellent in most cases

Contusion
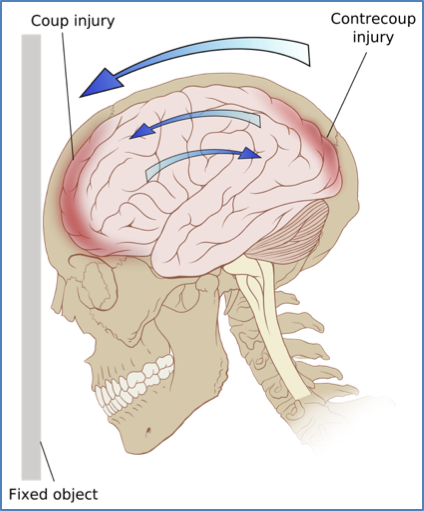
- Cause: High-force trauma (coup or contre-coup injury)
- Mechanism: Local bruising and swelling of brain parenchyma
- Clinical:
- Confusion, headache, dizziness
- Vomiting, seizures, cognitive/sensory deficits
- Investigations:
- CT/MRI → focal oedema, potential transtentorial herniation
- Management:
- ICU care, control raised ICP
- Avoid hypotension, hypercapnia, hyponatraemia
- Prognosis:
- Good recovery expected, though some memory/concentration issues may persist
Laceration
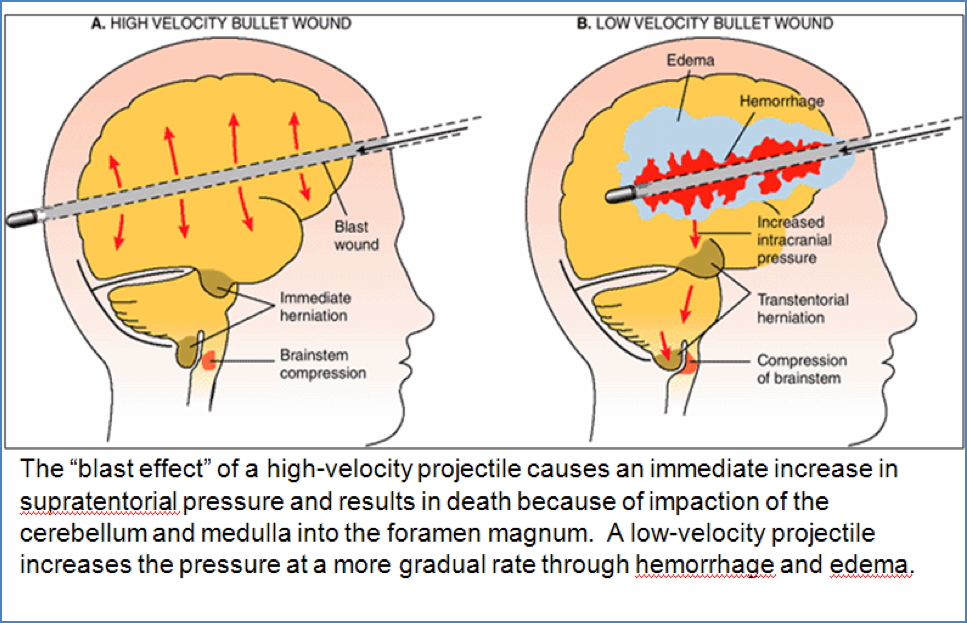
- Cause: Penetrating trauma (e.g. bullet, knife)
- Mechanism: Mechanical tearing of brain tissue
- Clinical:
- High velocity: instant death from brainstem herniation
- Low velocity: LOC, lucid interval possible, rising ICP
- Investigations:
- CT → visible laceration, haemorrhage, skull fractures
- Management:
- Prevent and manage raised ICP
- Prognosis:
- Poor, especially in high-velocity injuries
Diffuse Brain Injury
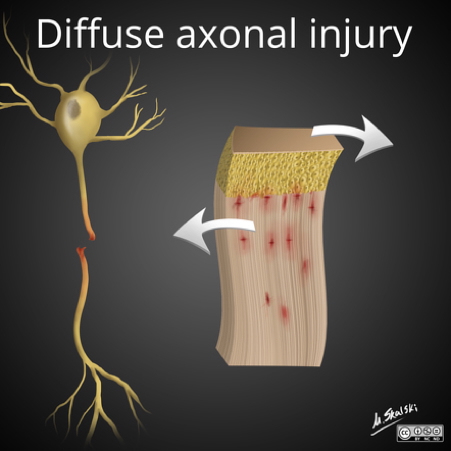
Diffuse Axonal Injury (DAI)
- Cause: High-speed trauma with rotational forces
- Mechanism: Shearing of axons, especially in corpus callosum and brainstem
- Clinical:
- Immediate unconsciousness
- Persistent vegetative state (90%)
- Severe mental impairment in survivors
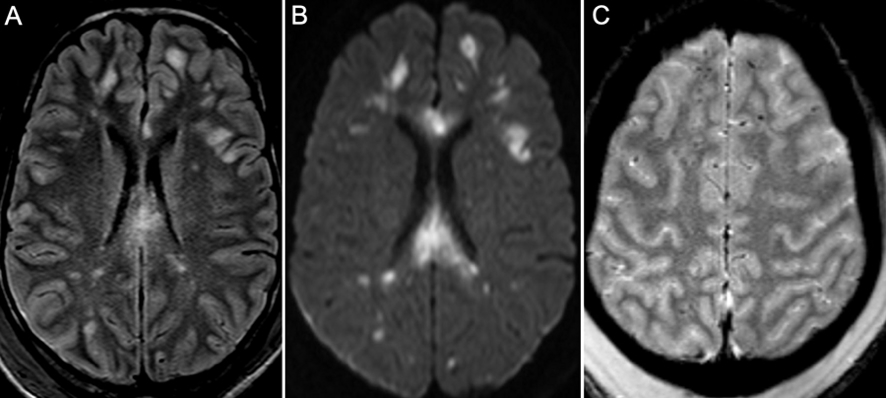
- Investigations:
- CT often normal initially
- MRI may reveal microhaemorrhages in deep brain structures
- Management:
- Supportive only; manage raised ICP
- Prognosis:
- Very poor (GCS 3 → high likelihood of organ donation)

Investigations
- Imaging:
- CT brain (first-line in most acute settings)
- MRI for subtle findings or delayed deterioration
- Clinical assessments:
- Glasgow Coma Scale
- Pupillary reflexes, neurological exam
- Lab tests:
- Rule out metabolic mimics (e.g. hypoglycaemia)
Management Overview
- Stabilise airway, breathing, circulation
- Monitor and manage intracranial pressure
- Neurosurgical referral when indicated (e.g. haematoma, herniation)
- Rehabilitation planning early in care
Complications
- Raised intracranial pressure
- Brain herniation
- Post-traumatic epilepsy
- Cognitive dysfunction
- Persistent vegetative state
- Psychological sequelae (e.g. depression, PTSD)
Differential Diagnosis
- Stroke (especially hemorrhagic)
- CNS infection (e.g. meningitis, encephalitis)
- Syncope or seizure with fall
- Hypoglycaemia or metabolic encephalopathy
Summary – Traumatic Brain Injuries
Traumatic brain injuries encompass a spectrum from mild concussions to devastating diffuse axonal injuries. Understanding the mechanism, clinical features, and imaging findings of focal versus diffuse injuries enables timely diagnosis and management. Always consider the possibility of raised intracranial pressure and the need for neuroimaging. For a broader context, see our Nervous System Overview page.