Table of Contents
Overview – Adaptive Immune System
The adaptive immune system is the body’s highly specialised third line of defence, targeting specific pathogens and generating long-term immunity. This system features remarkable specificity, memory, and self-tolerance, enabling it to eliminate threats with precision. Understanding how the adaptive immune system operates is essential for clinical reasoning in immunology, vaccination, and autoimmune disease management.
Definition
- The adaptive immune system (also known as the specific immune system) is the arm of the immune response that:
- Targets particular antigens with high specificity
- Responds systemically throughout the body
- Generates immune memory
- Self-limits once the pathogen is cleared
- Maintains self-tolerance, avoiding autoimmunity
Characteristics
- Specificity → Targets defined antigens
- Systemic activity → Not confined to infection site
- Memory → Faster and stronger upon re-exposure
- Self-limiting → Response fades after antigen elimination
- Self-tolerance → Avoids reaction against self-antigens
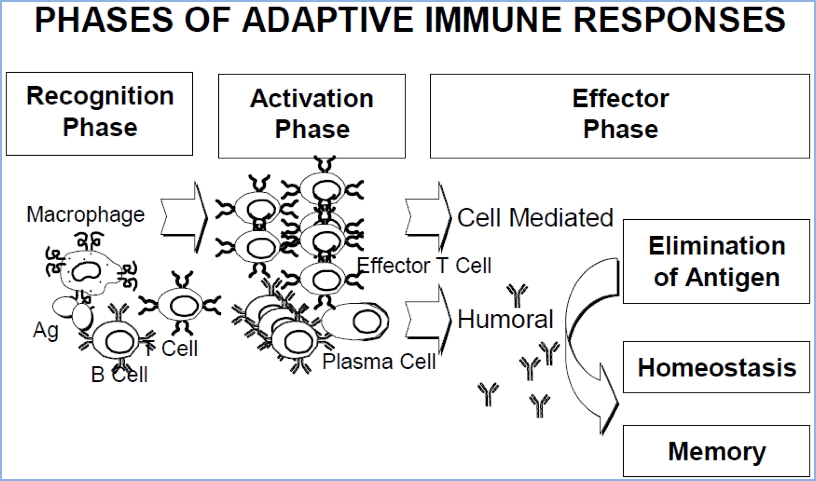
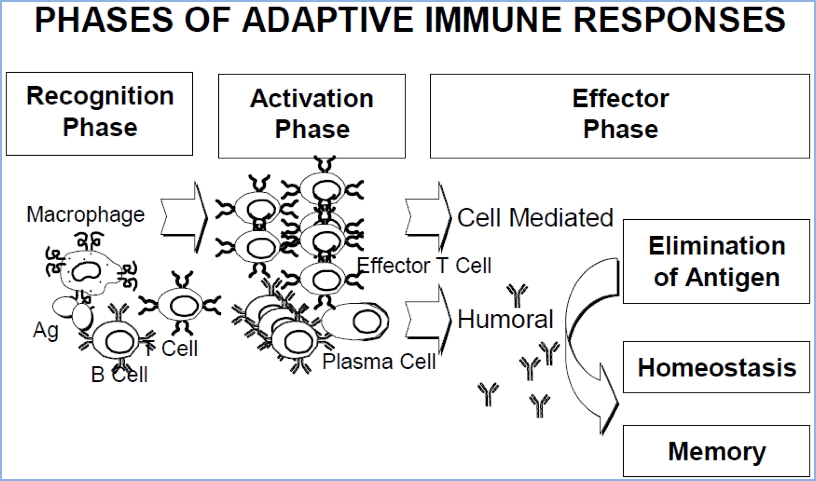
Phases of Adaptive Immunity
1. Recognition Phase
- Pathogen recognition via Toll-like receptors (TLRs) and pattern recognition receptors (PRRs)
- Macrophages and dendritic cells phagocytose pathogens, process antigens, and display them on MHC molecules
- Cytokines released from macrophages and injured epithelium recruit immune cells
2. Activation Phase
- Dendritic cells travel to local lymph nodes
- Activate naive T-cells, which in turn activate naive B-cells
- B-cells begin producing antibodies
3. Effector Phase
- Activated T-cells and secreted antibodies leave lymphoid tissue
- Enter circulation and migrate to the site of infection
Types of Adaptive Immunity
A. Cellular Immunity (T-Cell Mediated)
- Involves T-lymphocytes, macrophages, natural killer cells, and cytokines
- Effective against intracellular pathogens (e.g. viruses, some bacteria, cancer cells)
- Key features:
- T-cells induce apoptosis in infected cells
- NK cells and macrophages destroy infected or abnormal host cells
- Cytokines enhance local inflammation and immune activation


B. Humoral Immunity (Antibody-Mediated)
- Involves B-lymphocytes and immunoglobulins
- Targets extracellular microbes and toxins
- Key features:
- B-cells produce antibodies that circulate in blood and lymph
- Antibodies neutralise pathogens or mark them for phagocytosis
- Immunity can be transferred between individuals via serum
- Core mechanism behind vaccine effectiveness
- Secondary exposure → faster, higher antibody response due to memory B-cells


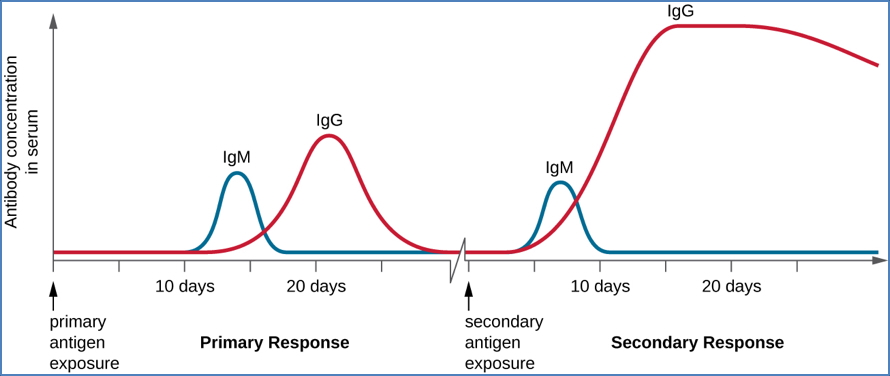
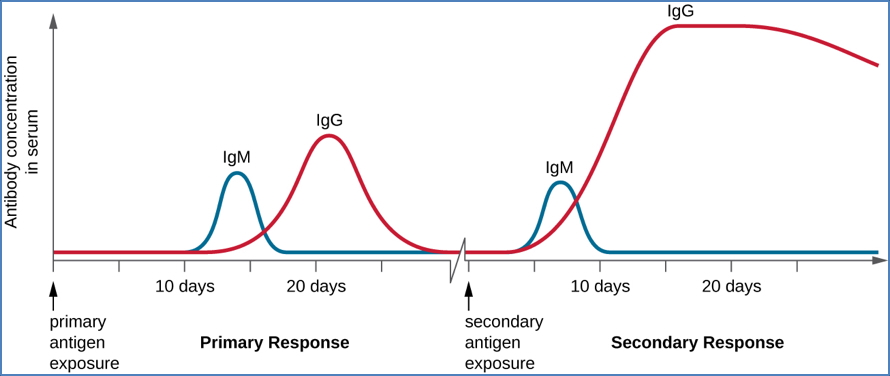
(Note: Once the body has Memory B-Cells from the first immune response, the immune reaction to the second exposure is much quicker and has a higher antibody yield. Is the primary mechanism behind vaccines)
Summary – Adaptive Immune System
The adaptive immune system is the body’s highly specific and memory-forming defence against infection. Divided into cellular and humoral branches, it enables targeted pathogen elimination and long-term immunity. Its functions are systemic, self-regulating, and essential to vaccine success. For a broader context, see our Immune & Rheumatology Overview page.