Table of Contents
Overview – Calcium & Phosphate Homeostasis
Calcium and phosphate are critical minerals involved in numerous physiological processes, including bone integrity, cellular metabolism, signal transduction, and neuromuscular function. The body maintains tight homeostatic control over their plasma levels via coordinated hormonal regulation involving parathyroid hormone, vitamin D, and calcitonin. Understanding calcium and phosphate homeostasis is essential for interpreting metabolic, renal, and endocrine disorders.
Definition
- Calcium and phosphate homeostasis refers to the regulation of plasma calcium and phosphate concentrations through absorption, excretion, and bone remodeling.
- Their balance is controlled by three main hormones: PTH, vitamin D (calcitriol), and calcitonin.
Functions
Calcium
- Structural functions:
- Skeletal development and maintenance.
- Biochemical functions:
- Intracellular signaling (second messenger).
- Neurotransmitter release (e.g. acetylcholine).
- Hormonal secretion.
- Muscle contraction.
- Blood clotting.
Phosphate
- Structural functions:
- Bone mineralization.
- Membrane phospholipid composition.
- Biochemical functions:
- Cellular energy (ATP hydrolysis).
- DNA/RNA backbone (phosphodiester bonds).
- Protein phosphorylation (signal transduction).
Magnesium (linked mineral)
- Structural role in bone (50% stored in bone).
- Biochemically essential for normal calcium levels.
- Renal Mg²⁺ reabsorption influenced by volume status, calcium, and plasma Mg²⁺ concentration.
Bone Chemistry
- Organic matrix (30% by weight):
- Primarily collagen (90%).
- Ground substance (10%).
- Inorganic mineral (70% by weight):
- Mainly hydroxyapatite: Ca₁₀(PO₄)₆(OH)₂.
- Bone serves as a rapid calcium buffer for plasma calcium levels.
Serum Concentrations
Calcium
- Plasma level tightly regulated at ~9.4 mg/dL (~2.4 mmol/L).
- ~99% stored in bone; ~1% extracellular.
- Circulates in 3 forms:
- 50% ionized (physiologically active).
- 10% covalently bound (diffusible).
- 40% protein-bound (non-diffusible, mainly to albumin).
Phosphate
- Loosely regulated at ~2.4–4.1 mg/dL.
- ~99% stored in bone; ~1% extracellular.
- Levels influenced by age, sex, diet, and calcium-regulating hormones.
Regulation of Plasma Calcium & Phosphate
Intestinal Absorption
- Calcium:
- Passive absorption is inefficient.
- Vitamin D dramatically increases absorption.
- PTH indirectly enhances absorption via vitamin D activation.
- Phosphate:
- Readily absorbed in the gut.
- Excess is excreted renally.
Renal Excretion
- Calcium:
- 99% filtered calcium is reabsorbed.
- 90% in PCT, Loop of Henle, and early DCT.
- 10% regulated in the late DCT.
- PTH enhances reabsorption (↓ urinary calcium loss).
- Calcitonin weakly increases calcium excretion.
- 99% filtered calcium is reabsorbed.
- Phosphate:
- Excreted via an overflow mechanism.
- PTH strongly increases phosphate excretion by inhibiting proximal tubular reabsorption.
Bone Remodeling
- PTH: Promotes osteoclast activity (resorption).
- Vitamin D: Supports mineral deposition.
- Calcitonin: Inhibits osteoclasts, favoring bone deposition (especially in children).
Hormonal Regulators
1. Parathyroid Hormone (PTH)
- Secreted by: Chief cells of parathyroid glands.
- Primary actions:
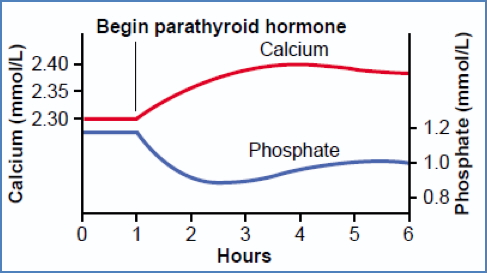
- ↑ Plasma calcium via:
- Bone resorption.
- Reduced renal calcium excretion.
- Enhanced vitamin D activation → ↑ intestinal absorption.
- ↓ Plasma phosphate via:
- Increased renal phosphate excretion.
- ↑ Plasma calcium via:
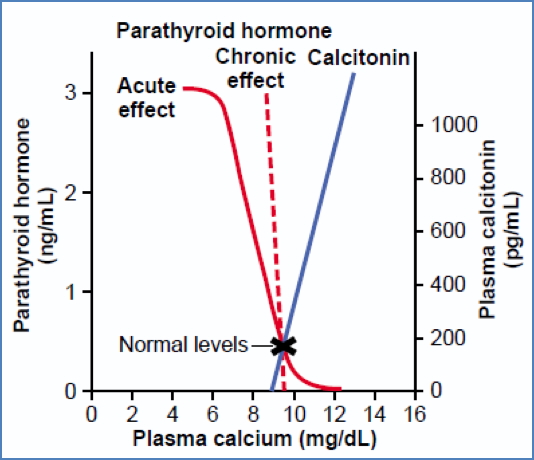
- Stimulated by: Low extracellular calcium.
- Inhibited by: High extracellular calcium, vitamin D.
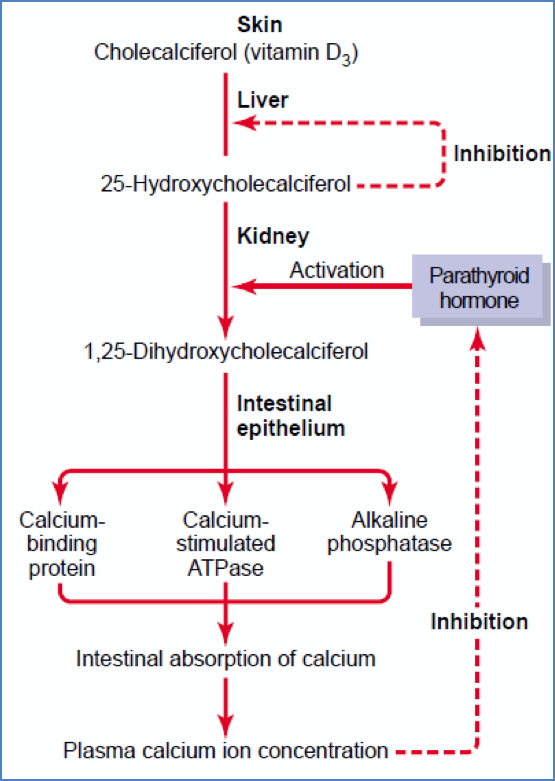
2. Vitamin D (Calcitriol)
- Active form: 1,25(OH)₂D₃.
- Activated by:
- Skin (UV exposure), liver, and kidneys (PTH-dependent final step).
- Primary actions:
- ↑ Intestinal absorption of calcium and phosphate.
- Supports PTH-mediated bone mobilization.
- At low levels, may promote bone mineralization.
- Negative feedback regulation: Plasma calcium suppresses PTH, indirectly controlling active vitamin D production.

3. Calcitonin
- Secreted by: Parafollicular cells (C cells) of thyroid.
- Primary actions:
- ↓ Plasma calcium by inhibiting osteoclasts.
- Effects more pronounced in children.
- Stimulated by: Elevated extracellular calcium.

Summary – Calcium & Phosphate Homeostasis
Calcium and phosphate homeostasis is maintained through a finely tuned balance of absorption, excretion, and bone remodeling under hormonal control by parathyroid hormone, vitamin D, and calcitonin. Disruptions in this balance lead to a variety of endocrine, metabolic, and skeletal disorders. For a broader context, see our Endocrine Overview page.
