Table of Contents
Overview – Procedural Dermatology
Procedural dermatology encompasses the hands-on surgical, diagnostic, and therapeutic techniques used in the treatment and management of various skin conditions. Final-year medical students must be familiar with key dermatological procedures including local anaesthesia, cryotherapy, biopsy methods, curettage, suturing, and advanced wound reconstruction with grafts or flaps. This page provides a high-yield overview of these essential interventions, equipping students for both clinical application and OSCE preparation.
Local Anaesthesia
Mechanism of Action
- Blocks voltage-gated sodium channels → inhibits nerve action potential conduction
- Rapid onset; vasodilatory effect shortens duration unless combined with adrenaline
Agents
- Lignocaine (1%)
- Onset: 1–5 minutes
- Duration: 30–120 minutes
- Max dose:
- 4 mg/kg without adrenaline
- 7 mg/kg with adrenaline
- Avoid use with adrenaline in end-artery locations (digits, penis) and long QT syndrome
- Ropivacaine (Naropin)
- Slower onset
- Longer acting
- Max dose: 2–3 mg/kg
- Topical
- Xylocaine gel (mucosa)
- ELMA cream (skin)
Nerve Blocks
- Digital block (ring block): 2% lignocaine, minimal volume
- Wrist block: targets radial, median, and ulnar nerves → full hand anaesthesia
Curettage & Electrocautery
- Used for:
- Warts, molluscum contagiosum, actinic keratoses
- Biopsy of nodular or superficial lesions
- Wound healing:
- Light curettage = few days
- Deeper lesions (e.g. on trunk) = 4–6 weeks
Cryotherapy
- Liquid nitrogen is the gold standard
- Indications
- Benign: molluscum, warts, seborrhoeic keratoses, skin tags
- Premalignant: actinic keratoses, actinic cheilitis
- Malignant: superficial BCC
Expected Effects
- Pain, oedema, vesicles, crusting
- Temporary adverse effects: hypo/hyperpigmentation, infection
- Permanent risks: scarring, alopecia, nail dystrophy
Biopsy Techniques
- Punch biopsy: minimal scarring; ideal for face
- Shave biopsy: simple, best for bulky lesions
- Curette biopsy: fast, minimal tools
- Incisional biopsy: deeper ellipse sample, ideal for diagnosis
- Excisional biopsy: removes entire lesion, provides full pathology sample
Wound Design
- Align incisions with relaxed skin tension lines
- Excision margins:
- Benign: 2–5 mm
- Malignant: up to 2 cm depending on tumour
Surgical Wound Repair
Suture Materials
- Non-absorbable synthetic: Nylon, polypropylene (external use)
- Absorbable synthetic: Monocryl, Vicryl (internal; hydrolysis breakdown)
- Non-synthetic:
- Absorbable: catgut (obsolete)
- Non-absorbable: silk
Suture Size
- Scale 1–6:
- 1 = thinnest (0.4 mm)
- 2 = thickest (0.8 mm)
Repair Types
- Primary repair: within 6–8 hours
- Delayed primary repair: 72 hours post-cleaning
- Secondary intention: >72 hours, clean environment
Pre-requisites
- Clean wound
- Eliminate dead tissue/space
- Use minimal tension
- Timely suture removal (typically within 1–2 weeks)
Skin Grafts vs Skin Flaps
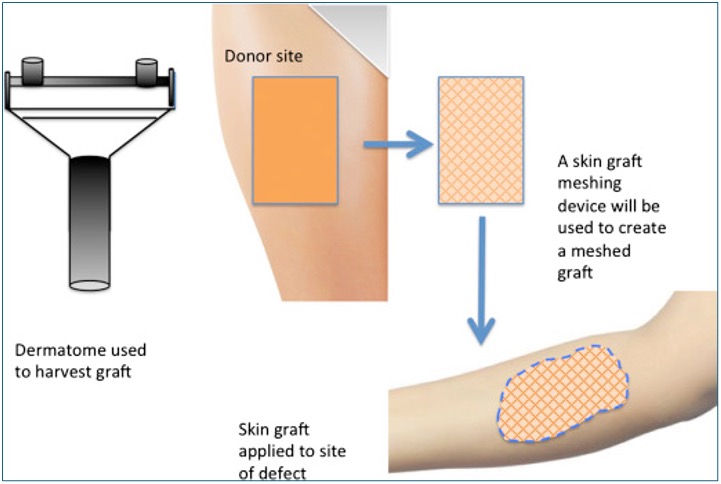
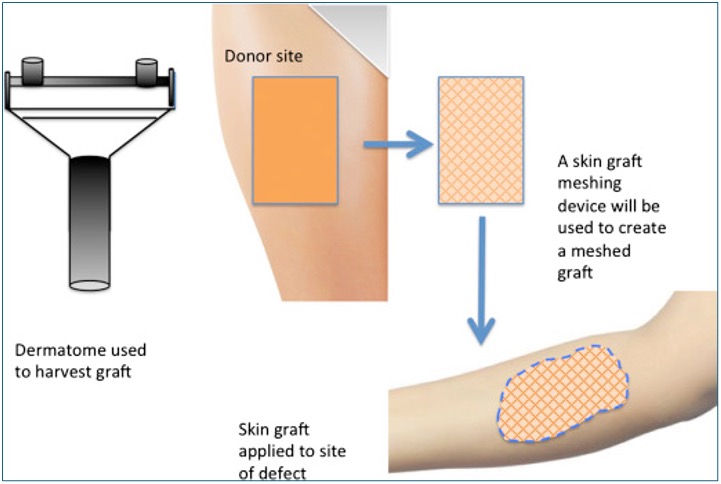
Skin Grafts
- Fully detached → lacks intrinsic blood supply
- Types:
- Full thickness graft (FTG): dermis + epidermis
- Split skin graft (SSG): epidermis + superficial dermis
- Survive initially by diffusion; long-term via neovascularisation
Skin Flaps
- Not fully detached → maintains blood supply
- Indications:
- Poor vascularity (bare bone, tendons)
- Cosmetic priority (face)
- Vital structures (vessels, joints)
- Types:
- Rotation
- Advancement
- Transposition
- Free flaps: transferred tissue with microsurgical reconnection of vessels


Summary – Procedural Dermatology
Procedural dermatology covers a broad range of essential surgical and therapeutic skills, from local anaesthesia and biopsy techniques to cryotherapy and skin reconstruction. These skills are central to dermatological practice and often overlap with minor surgical procedures. For a broader context, see our Skin & Dermatology Overview page.