Table of Contents
Overview – Testicular Physiology
Testicular physiology refers to the hormonal and cellular processes that drive spermatogenesis and testosterone production within the testes. This includes the coordinated actions of Sertoli and Leydig cells, the seminiferous tubules, and the brain-testicular axis. Understanding these processes is crucial in clinical contexts such as male infertility, hypogonadism, and hormone-responsive cancers.
Definition
Testicular physiology encompasses the function of the testes, primarily involving:
- Spermatogenesis: the production and maturation of sperm
- Hormone production: especially testosterone, under endocrine regulation
Spermatogenesis
Occurs within the seminiferous tubules and involves several stages:
- Spermatogonia (2n)
- Stem cells in contact with the basal lamina
- Divide by mitosis to produce:
- Type A: Remains as stem cells for future division
- Type B: Becomes a primary spermatocyte
- Primary Spermatocyte (2n)
- Undergoes meiosis I → forms two secondary spermatocytes (haploid)
- Secondary Spermatocyte (n)
- Undergoes meiosis II → produces four spermatids
- Spermatids (n)
- Small, round, large-nucleated cells near the lumen
- Non-motile and immature
- Spermiogenesis (morphological transformation)
- Spermatids elongate
- Shed excess cytoplasm
- Form flagella → mature spermatozoa
- Spermatozoa
- Head:
- Flattened nucleus with compacted DNA
- Acrosome (enzyme-containing cap for egg penetration)
- Mid-piece:
- Mitochondria spiral around flagellar base
- Tail:
- Whip-like flagellum enables motility (once activated by prostatic fluid)
- Head:


Sertoli Cells (Sustentacular Cells)
- Extend from the basal lamina to the tubule lumen
- Functions:
- Support and nourish developing sperm
- Respond to FSH by releasing androgen-binding protein (ABP)
- Secrete inhibin (involved in feedback inhibition of FSH)
- Form the blood-testis barrier via tight junctions
- Creates basal vs adluminal compartments
- Prevents sperm antigens from entering systemic circulation
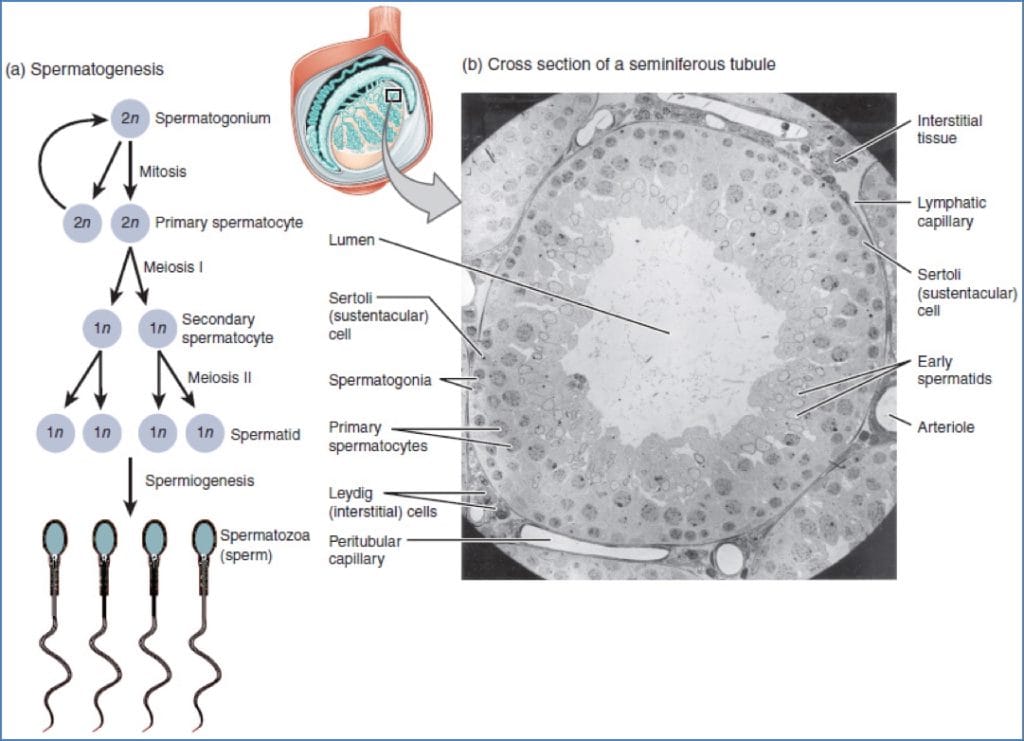
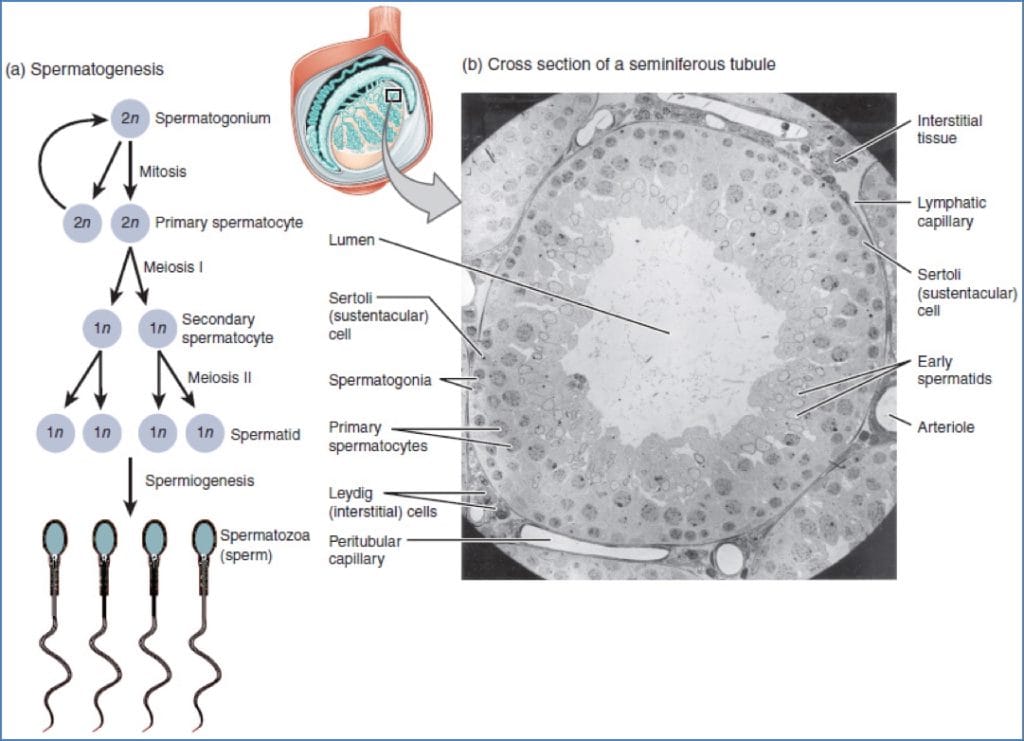
Leydig Cells
- Located in the interstitial space (outside seminiferous tubules)
- Stimulated by LH
- Produce testosterone, which is essential for:
- Initiation and maintenance of spermatogenesis
- Secondary male sexual characteristics
Neuroendocrine Regulation – Brain-Testicular Axis
A finely tuned feedback system involving the hypothalamus, pituitary gland, and testes:
- GnRH (Gonadotropin-Releasing Hormone)
- Secreted by the hypothalamus
- Stimulates the anterior pituitary to release FSH and LH
- FSH (Follicle Stimulating Hormone)
- Stimulates Sertoli cells
- Promotes production of ABP, which binds testosterone to promote sperm maturation
- LH (Luteinising Hormone)
- Stimulates Leydig cells
- Increases testosterone production
- Testosterone
- Maintains spermatogenesis
- Exerts negative feedback on the hypothalamus → ↓ GnRH
- High testosterone levels → ↓ LH and FSH
- Inhibin
- Secreted by Sertoli cells
- Specifically inhibits FSH release → fine-tunes sperm production
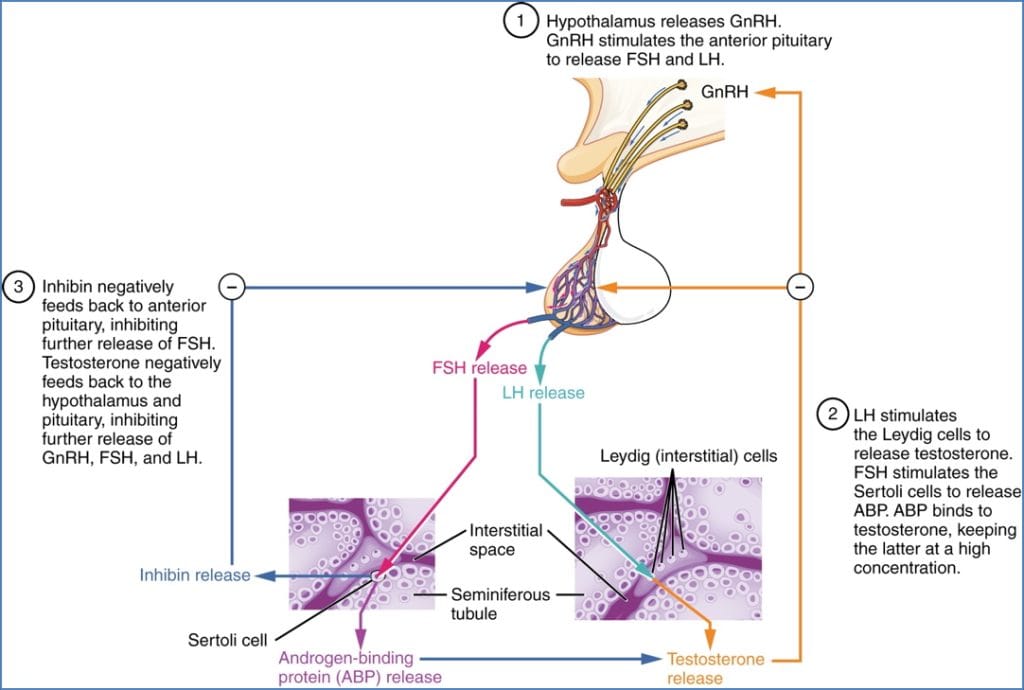
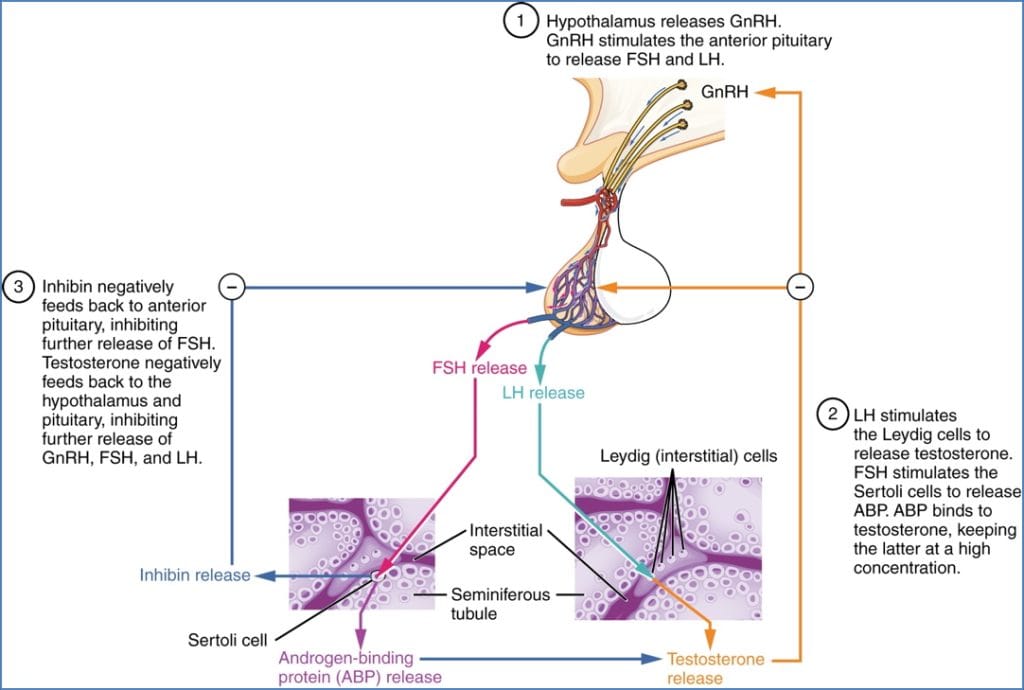
Feedback Loop Summary
- High sperm count (>20 million/mL):
- ↑ Inhibin and testosterone → ↓ GnRH → ↓ FSH/LH → ↓ testosterone → ↓ spermatogenesis
- Low sperm count (<20 million/mL):
- ↓ Inhibin and testosterone → ↑ GnRH → ↑ FSH/LH → ↑ testosterone and ABP → ↑ spermatogenesis
Summary – Testicular Physiology
Testicular physiology involves spermatogenesis and hormone regulation, orchestrated by Sertoli and Leydig cells under the influence of the hypothalamic-pituitary-gonadal axis. Hormones such as FSH, LH, testosterone, and inhibin regulate sperm production through a negative feedback loop. For a broader context, see our Reproductive Health Overview page.