Table of Contents
Overview – Congenital Penile Abnormalities
Congenital penile abnormalities are structural anomalies of the penis present from birth. These can impact urinary function, sexual development, and fertility, and range in severity from minor cosmetic concerns to urological emergencies. Early diagnosis and appropriate surgical or medical management are crucial to prevent long-term complications such as infections, infertility, or psychosocial distress. This page outlines the key congenital penile abnormalities including phimosis, paraphimosis, hypospadias, epispadias, and penile agenesis.
Definition
Congenital penile abnormalities refer to anatomical malformations of the penis or its associated structures, arising due to defective embryological development.
Aetiology
- Congenital malformations of the penis and urethra
- Genetic or hormonal causes: e.g., androgen insensitivity or lack of testosterone production
- Secondary scarring or fibrosis due to infections (in acquired phimosis and paraphimosis)
Types of Congenital Penile Abnormalities
Phimosis
What?
- Inability to retract the foreskin over the glans penis
Why?
- Often congenital
- May be acquired due to repeated infections → fibrosis and scarring of the preputial ring
Outcome?
- Can cause hygiene issues → secondary infections, balanitis
- Chronic inflammation may → penile carcinoma if untreated
Paraphimosis
What?
- Retracted foreskin becomes trapped behind the glans penis and cannot be returned
Why?
- Can follow congenital or acquired phimosis
- Occurs when foreskin is left retracted too long → becomes oedematous and stuck
Outcome?
- Urological emergency: may → venous congestion, ischaemia, gangrene, and eventual loss of penile tissue
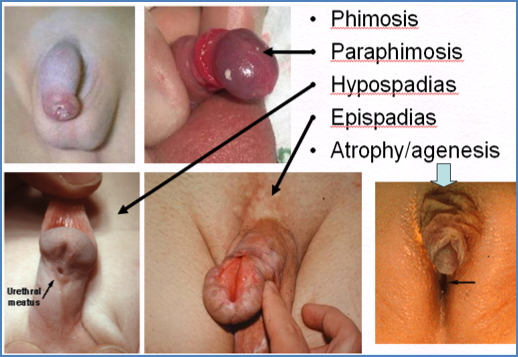
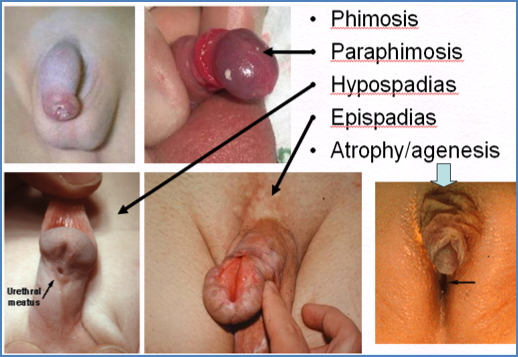
Hypospadias & Epispadias
What?
- Hypospadias: Urethral opening is located on the ventral (underside) surface of the penis
- Epispadias: Urethral opening is on the dorsal (upper) surface
- Hypospadias is far more common
Why?
- Congenital defect in urethral groove formation
- Often associated with other abnormalities like cryptorchidism
Outcome?
- Impaired urinary stream and direction → risk of UTI
- May cause abnormal ejaculation, erectile issues, and fertility problems


Penile Atrophy / Agenesis
What?
- Complete or partial absence of penile development
Why?
- Rare congenital condition (≈1 in 6 million births)
- Frequently linked to testicular agenesis → absent testosterone exposure during development
Outcome?
- No urinary outlet → requires surgical creation of urethral opening
- If testes are present: normal male secondary sexual characteristics
- If testes absent: no puberty → maintained pre-pubescent appearance
Clinical Features
- Cosmetic or structural abnormality at birth
- Abnormal urination or urinary stream
- Inability to retract foreskin (phimosis) or return it (paraphimosis)
- Signs of infection, redness, or swelling
- In severe cases: urinary retention or necrosis
Investigations
- Clinical examination is usually sufficient
- Ultrasound or genetic testing if concerned about underlying disorders of sex development (DSDs)
- Voiding cystourethrogram (VCUG) in complex hypospadias or suspected reflux
Management
Phimosis
- Observation in infants (often resolves naturally)
- Topical steroid creams
- Circumcision if symptomatic or persistent
Paraphimosis
- Emergency manual reduction
- Dorsal slit or circumcision if reduction fails
Hypospadias & Epispadias
- Surgical correction (usually age 6–18 months)
- Avoid neonatal circumcision to preserve tissue for repair
- Long-term follow-up for urinary or sexual complications
Penile Agenesis
- Urological and surgical management to create functional urinary outlet
- Hormonal replacement therapy if testicular agenesis present
- Psychological support and counselling
Complications
- Chronic urinary tract infections
- Erectile or fertility issues
- Psychosocial distress
- Ischaemia or necrosis in untreated paraphimosis
- Poor self-image or stigma in adolescence
Summary – Congenital Penile Abnormalities
Congenital penile abnormalities include phimosis, paraphimosis, hypospadias, epispadias, and penile agenesis. These malformations range from benign conditions to surgical emergencies and can significantly impact urinary, sexual, and psychosocial function. Timely recognition and referral are essential. For a broader context, see our Reproductive Health Overview page.