Table of Contents
Overview – Membranous Nephropathy
Membranous Nephropathy (also known as Membranous Glomerulonephritis or MGN) is the leading cause of adult-onset nephrotic syndrome, responsible for over 50% of cases. It typically presents in middle-aged adults with oedema, proteinuria, and preserved renal function in the early stages. The condition arises from immune complex deposition in the glomerular basement membrane, leading to progressive glomerular damage. Prompt diagnosis and risk-stratified treatment are crucial to avoid progression to end-stage renal disease (ESRD).
Definition
Membranous Nephropathy is a chronic immune-mediated glomerulopathy characterised by:
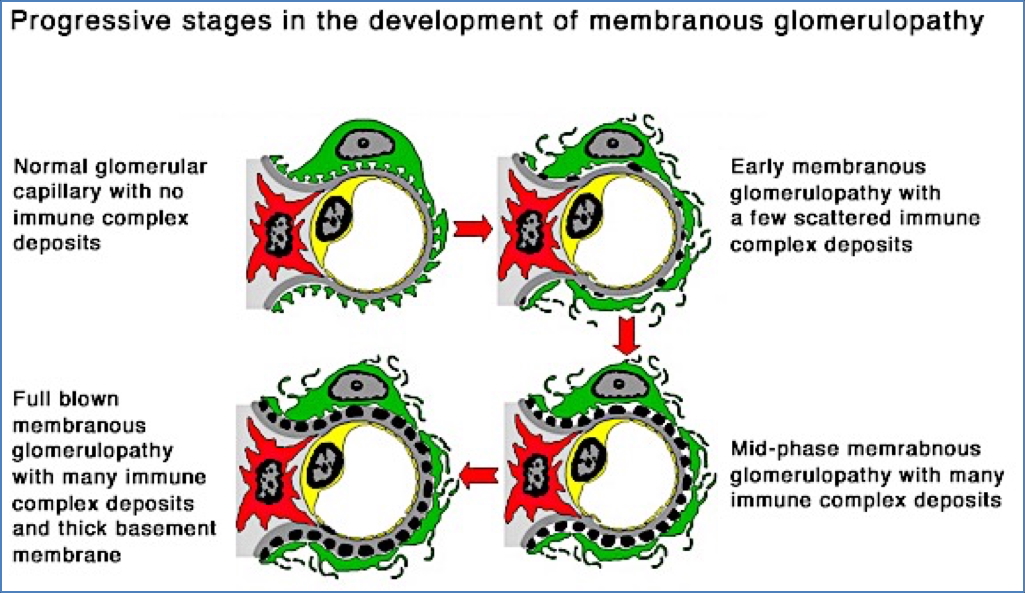
- Subepithelial immune complex deposition along the glomerular basement membrane (GBM)
- Nephrotic-range proteinuria
- Thickened GBM without significant cellular proliferation
Aetiology
- Idiopathic (Primary) – most common
- Secondary causes:
- Infections: Hepatitis B, Hepatitis C, Syphilis
- Autoimmune: Systemic Lupus Erythematosus (SLE)
- Drugs: NSAIDs
- Malignancies: Solid organ tumours (especially lung, colon)
Pathophysiology
- Formation of antigen–antibody complexes (either circulating or in situ)
- → Deposit along the subepithelial surface of the GBM
- → Activation of complement pathway
- → Inflammatory injury to podocytes and mesangial cells
- → Increased permeability of GBM → massive proteinuria → nephrotic syndrome
Clinical Features
- Most common in adults aged 40–60 years
- Often insidious onset
- Classic presentation:
- Oedema (especially periorbital and lower limbs)
- Frothy urine (due to proteinuria)
- Fatigue, malaise
- Preserved renal function initially
- Case example: 35-year-old woman with leg swelling and puffy eyelids, worsening over two months.
Investigations
- Urinalysis:
- Nephrotic-range proteinuria (>3.5g/day)
- Microscopy typically bland
- Bloods:
- Hypoalbuminaemia
- Hyperlipidaemia
- Mildly raised creatinine (in later stages)
- Renal Biopsy:
- Light microscopy: Thickened GBM
- Immunofluorescence: granular IgG and C3 deposits
- Electron microscopy: Subepithelial immune deposits
Management
- Supportive Therapy:
- Diuretics (e.g. frusemide) for oedema
- ACE inhibitors to reduce proteinuria and control BP
- Heparin in selected cases to prevent thrombosis
- Salt and fat intake reduction
- Disease-Modifying Treatment:
- Treat underlying cause (e.g. hepatitis, malignancy)
- Immunosuppression:
- Prednisone ± cyclophosphamide or ciclosporin for high-risk patients
- Rituximab increasingly used in resistant or relapsing cases
Prognosis
- Spontaneous complete remission: 5–30% within 5 years
- Spontaneous partial remission: 25–40%
- Progression to ESRD: Occurs in a minority (risk correlates with degree of proteinuria and renal impairment)
Complications
- Progressive chronic kidney disease
- Thromboembolism (loss of antithrombin-III)
- Infection risk (loss of immunoglobulins)
- Relapse or steroid-resistance in some patients
Differential Diagnosis
- Minimal Change Disease
- Focal Segmental Glomerulosclerosis (FSGS)
- Diabetic Nephropathy
- Lupus Nephritis (especially Class V)
Summary – Membranous Nephropathy
Membranous Nephropathy is the leading cause of nephrotic syndrome in adults, with a broad range of potential causes including autoimmune disease, infection, and malignancy. Diagnosis is confirmed via renal biopsy, and treatment is guided by severity and risk of progression. For further nephrotic and renal pathology topics, explore our Renal Overview page.