Table of Contents
Overview – Lipid Lowering Drugs
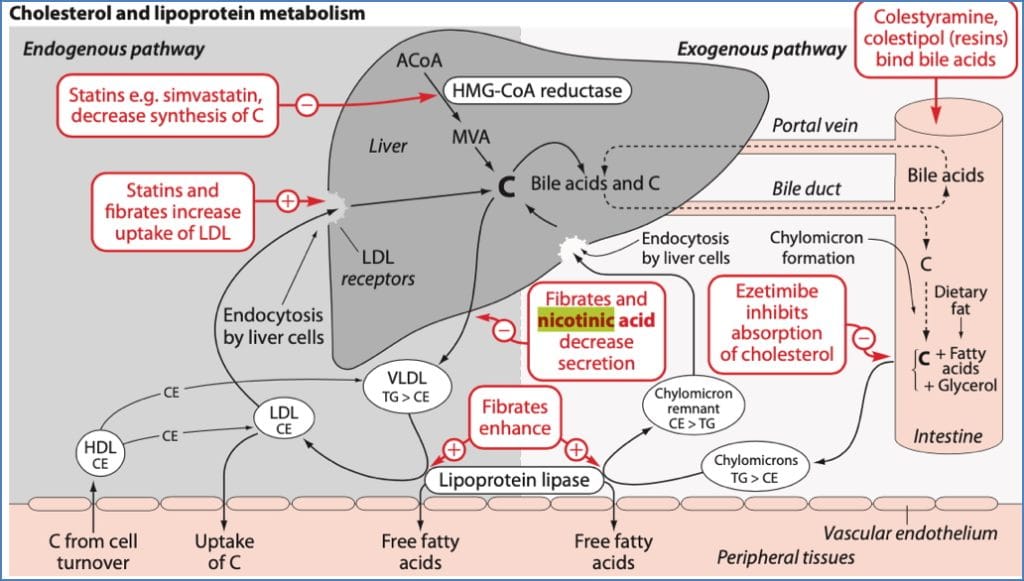
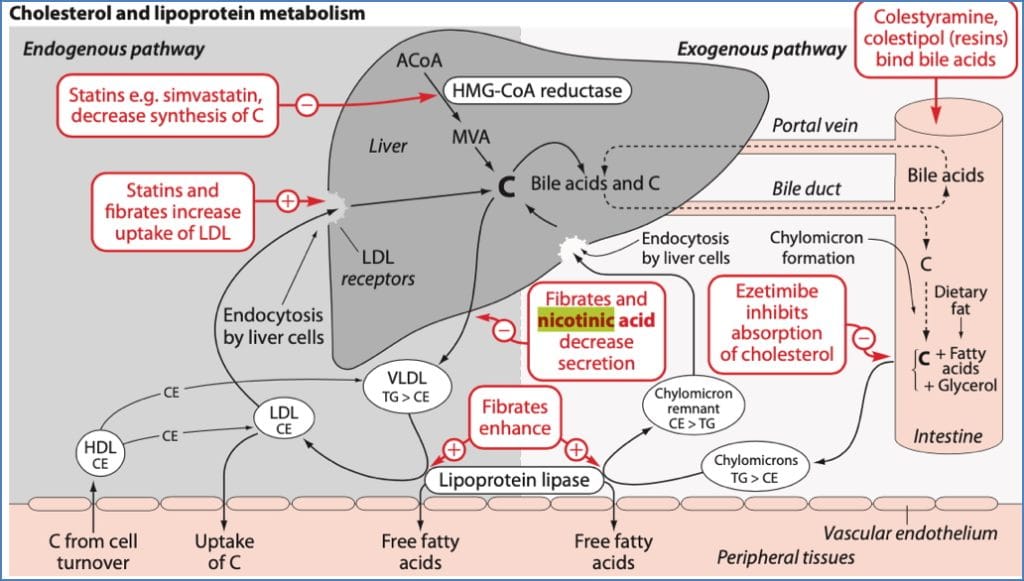
Lipid lowering drugs are a cornerstone in the management of hypercholesterolaemia and hyperlipidaemia, both of which are significant risk factors for atherosclerosis and cardiovascular disease. These medications work through various mechanisms to reduce low-density lipoprotein (LDL), triglycerides, and sometimes increase high-density lipoprotein (HDL). They are often initiated alongside or following lifestyle changes when patients are at elevated cardiovascular risk.
Definition
Lipid lowering drugs are a group of medications used to reduce serum lipid levels, particularly LDL cholesterol and triglycerides. They help prevent atherosclerotic cardiovascular diseases, including myocardial infarction and stroke.
Indications
- Primary and secondary prevention of atherosclerotic cardiovascular disease (ASCVD)
- Familial hypercholesterolaemia
- Hypertriglyceridaemia
- Mixed dyslipidaemia
- Acute coronary syndrome (as part of secondary prevention)
Classes of Lipid Lowering Drugs
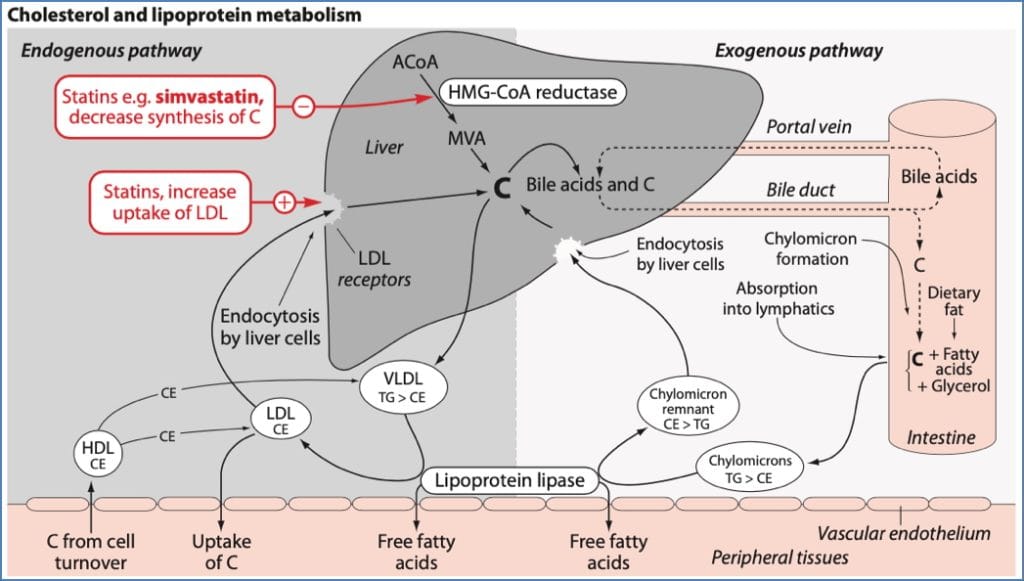
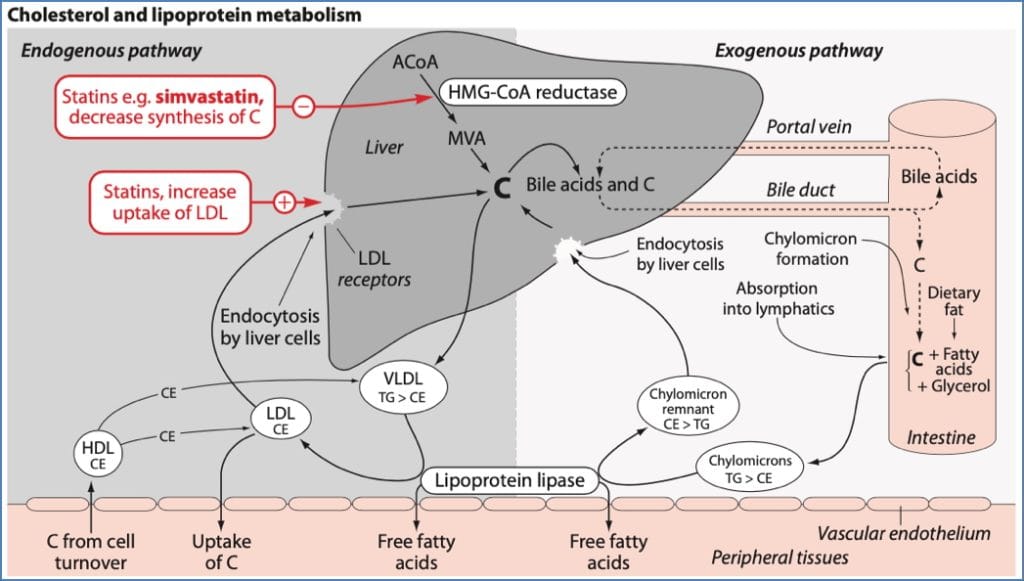
1. Statins – HMG-CoA Reductase Inhibitors
Classical Agents:
- Simvastatin
- Fluvastatin
- Pravastatin
- Lovastatin
Note: These are fungal derivatives (Aspergillus), which can trigger immune-related adverse effects.
Mechanism of Action:
- Inhibit HMG-CoA reductase, the rate-limiting enzyme in cholesterol synthesis (converts HMG-CoA → mevalonate)
- ↓ Endogenous cholesterol synthesis
- ↑ LDL-receptor expression in hepatocytes → ↑ LDL clearance from plasma
- Additional anti-inflammatory effects on arterial walls may reduce atherosclerotic risk
Side Effects:
- Myositis → ↑ Creatine Kinase
- Can progress to rhabdomyolysis
- Immune-related adverse effects due to fungal origin
2. Ion Exchange Resins – Bile Acid-Binding Resins
Classical Agents:
- Colestyramine
- Colestipol
Mechanism of Action:
- Bind bile acids and dietary cholesterol in the gut → prevent reabsorption
- Stimulate hepatic LDL receptor upregulation to compensate for bile loss → ↑ LDL clearance
- ↓ Total blood cholesterol
Side Effects:
- Malabsorption of fat-soluble vitamins (A, D, E, K) and folate
- Constipation – often requires concurrent laxatives
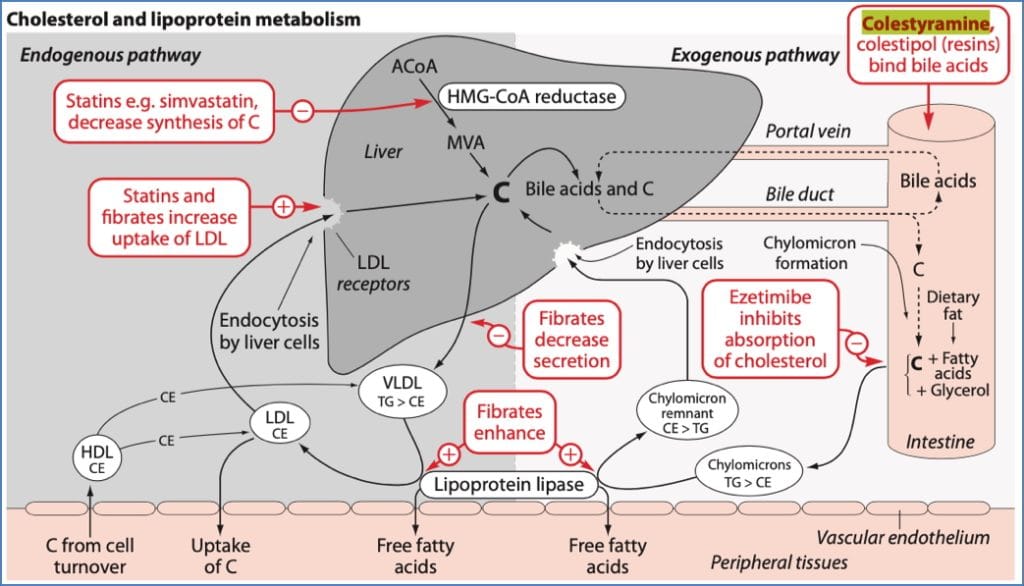
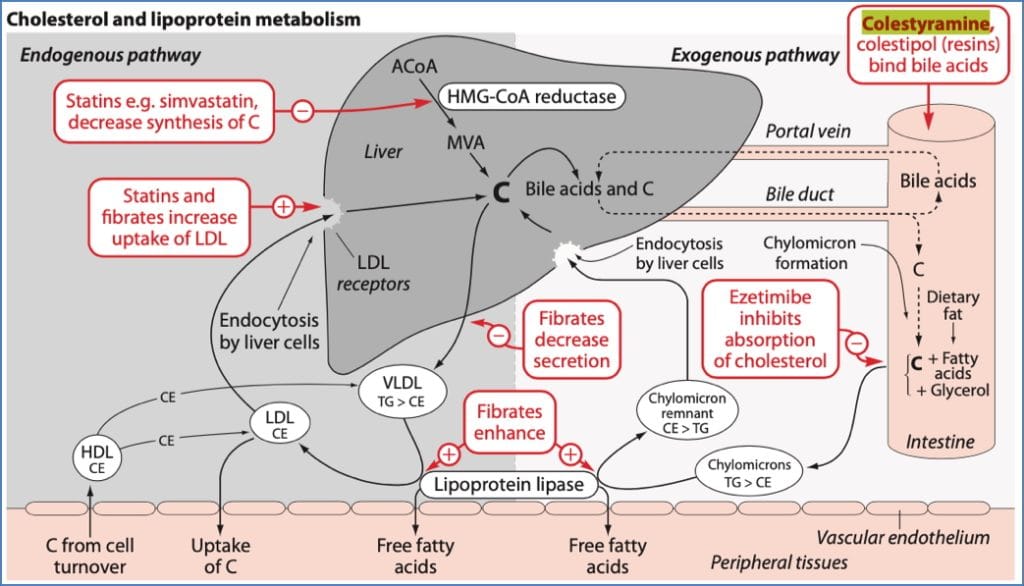
3. Ezetimibe
Mechanism of Action:
- Blocks cholesterol absorption at the brush border of the small intestine (specifically the duodenum)
Side Effects:
- Diarrhoea
- Abdominal pain
- Headache
- Avoid in lactating women (passes into breast milk)


Treating Hyperlipidaemia
4. Fibrates
Classical Agents:
- Clofibrate
- Gemfibrozil
- Fenofibrate
- Bezafibrate
- Ciprofibrate
Mechanism of Action:
- Activate PPAR-α →
- ↑ transcription of lipoprotein lipase
- ↑ conversion of VLDL to LDL
- ↓ VLDL production
- ↑ hepatic LDL uptake
Net effect: Marked ↓ in VLDL/triglycerides, modest ↓ LDL, and mild ↑ HDL
Side Effects:
- Myositis
- ↑ bile production → may cause gallstones
- Rare: Renal failure


5. Nicotinic Acid (Niacin) – Last-Resort Therapy
Mechanism of Action:
- ↓ Hepatic production of VLDL
- ↓ Conversion of VLDL to LDL
Side Effects:
- Requires very high doses, often poorly tolerated
- Causes flushing and palpitations → mitigated with co-administered aspirin
- Can impair liver function
- Alters glucose tolerance
- May trigger gout
Summary – Lipid Lowering Drugs
Lipid lowering drugs play a critical role in reducing cardiovascular risk through their effects on cholesterol and triglyceride levels. Statins remain first-line for most patients, while bile acid resins, ezetimibe, fibrates, and niacin provide additional or alternative mechanisms depending on lipid profile and tolerability. For a broader context, see our Pharmacology & Toxicology Overview page.
| Drug Class | Primary Effect | Key Side Effects |
|---|---|---|
| Statins | ↓ LDL (via ↓ synthesis + ↑ clearance) | Myositis, rhabdomyolysis, immune reactions |
| Ion Exchange Resins | ↓ LDL (via ↓ reabsorption + ↑ clearance) | Constipation, ↓ fat-soluble vitamin uptake |
| Ezetimibe | ↓ LDL (via ↓ intestinal absorption) | GI upset, headache, avoid in breastfeeding |
| Fibrates | ↓ VLDL (also ↓ LDL, ↑ HDL) | Myositis, gallstones, rare renal issues |
| Niacin | ↓ VLDL & LDL, ↑ HDL | Flushing, liver impairment, gout, hyperglycaemia |