Table of Contents
Overview – Gastrointestinal Drugs
Gastrointestinal drugs encompass a diverse group of agents that manage nausea, vomiting, constipation, and diarrhoea. These include anti-emetics targeting the chemoreceptor trigger zone (CTZ), laxatives for bowel regulation, and anti-motility agents for diarrhoea. Understanding the pharmacological classes, mechanisms, and clinical indications of gastrointestinal drugs is essential for final-year medical students.
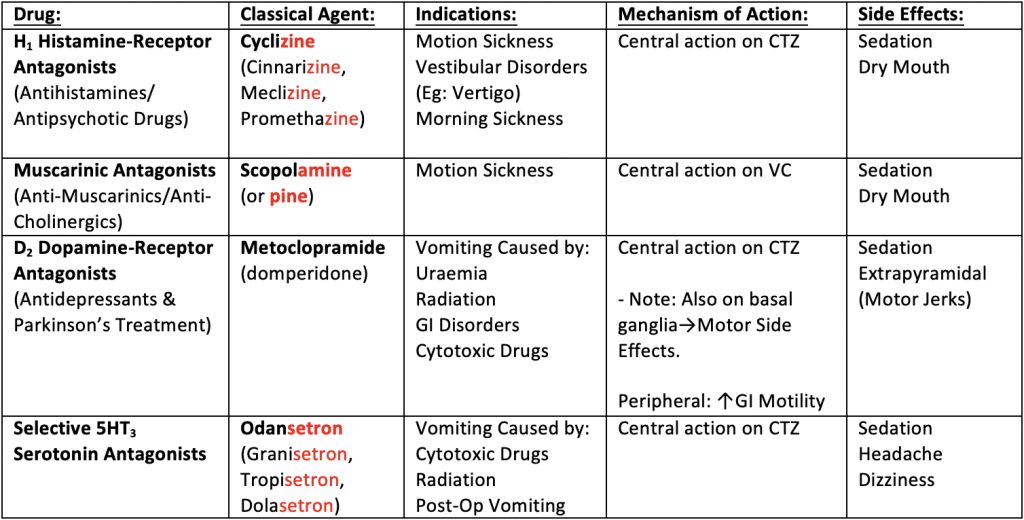
Anti-Emetic Drugs
Anti-emetics work primarily on the chemoreceptor trigger zone (CTZ) and vomiting centre (VC) in the medulla. They act by blocking neurotransmitter receptors involved in the emetic reflex.
Receptor Targets for Vomiting Reflex
- Histamine → H₁ receptor
- Acetylcholine → Muscarinic (M) receptor
- Dopamine → D₂ receptor
- Serotonin (5-HT) → 5-HT₃ receptor
- Enkephalins (Opioids) → Opioid receptors
Key Classes of Anti-Emetics
H₁ Histamine Receptor Antagonists
- Examples: Cyclizine, Cinnarizine, Meclizine, Promethazine
- Indications: Motion sickness, vestibular disorders, morning sickness
- Mechanism: Central inhibition of CTZ via histamine blockade
- Side Effects: Sedation, dry mouth
Muscarinic Antagonists (Anti-Cholinergics)
- Example: Scopolamine
- Indications: Motion sickness
- Mechanism: Inhibits VC centrally via muscarinic blockade
- Side Effects: Sedation, dry mouth
D₂ Dopamine Receptor Antagonists
- Examples: Metoclopramide, Domperidone
- Indications: Vomiting due to uraemia, GI disorders, radiation, chemotherapy
- Mechanism:
- Central: D₂ antagonism in CTZ
- Peripheral: Increases GI motility
- Note: Acts on basal ganglia → potential for extrapyramidal side effects
- Side Effects: Sedation, motor disturbances (e.g. dystonia, tremors)
5-HT₃ Serotonin Receptor Antagonists
- Examples: Ondansetron, Granisetron, Tropisetron, Dolasetron
- Indications: Chemotherapy-induced vomiting, radiation, post-op nausea
- Mechanism: Inhibits CTZ centrally via serotonin receptor blockade
- Side Effects: Sedation, headache, dizziness

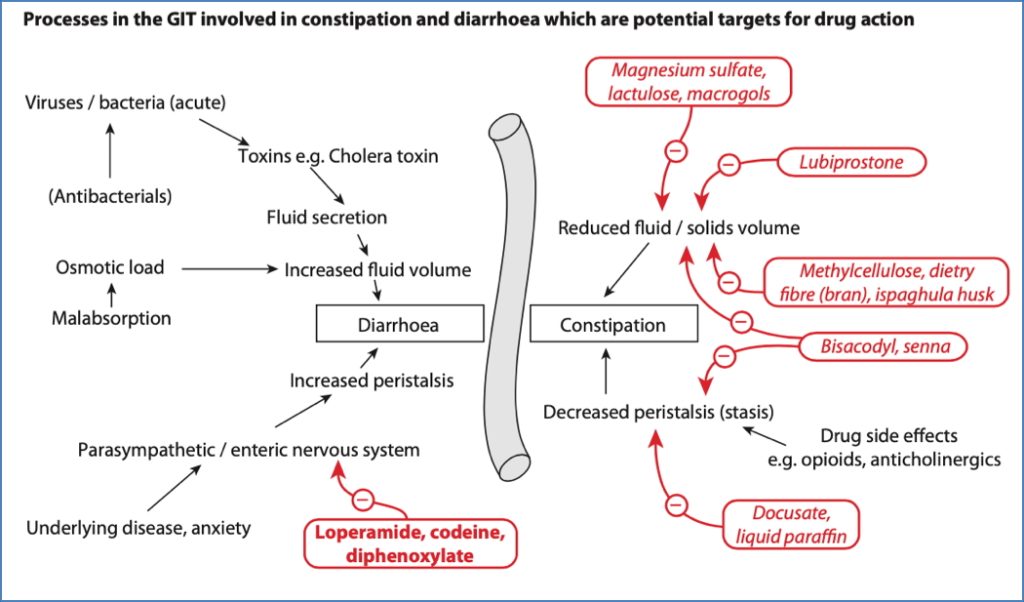
Laxatives
Laxatives are used to manage constipation by altering stool consistency and/or bowel motility.
Bulk-Forming Laxatives
- Examples: Methylcellulose, Bran, Husk
- Mechanism:
- Indigestible fibres → swell into a hydrated mass in the gut lumen
- ↑ Peristalsis via mechanical stretch
- Side Effects: Generally safe, no major side effects
Osmotic Laxatives
- Examples: Lactulose, Macrogols
- Mechanism:
- Poorly absorbed solutes increase luminal osmolarity → water retention
- Distension of bowel leads to purgation
- Side Effects: Abdominal cramps, vomiting
Stimulant Laxatives
- Example: Docusate
- Mechanism:
- Stimulate electrolyte and water secretion by intestinal mucosa
- Stimulate enteric nerves → increased peristalsis
- Side Effects: Abdominal cramps
Anti-Motility / Spasmolytic Agents
These are used to reduce bowel motility in diarrhoea.
Opioids
- Examples: Loperamide, Codeine
- Mechanism:
- ↑ GI tone and rhythmic contractions
- ↓ Propulsive activity (ileocolic and anal sphincters)
- Note: Loperamide does not cross the blood-brain barrier → non-addictive
Adsorbents
- Examples: Chalk, Charcoal, Silicates
- Mechanism:
- Symptomatic relief via adsorption of microorganisms/toxins
- Form protective layer on intestinal mucosa
- Precise mechanism unclear
Summary – Gastrointestinal Drugs
Gastrointestinal drugs include anti-emetics, laxatives, and anti-diarrhoeal agents that target specific receptors and physiological pathways to relieve symptoms of nausea, vomiting, constipation, and diarrhoea. Anti-emetics work on CTZ and VC via histamine, dopamine, serotonin, and muscarinic pathways, while laxatives and opioids modulate intestinal motility and fluid content. For a broader context, see our Pharmacology & Toxicology Overview page.