Table of Contents
Overview – Drug Administration
Drug administration is a core pharmacological concept that influences how effectively a drug reaches its target and exerts its intended effect. Understanding the different administration routes, drug distribution patterns, metabolism, and excretion is vital for safe and effective prescribing. Medical students must also grasp how pharmacokinetics and pharmacodynamics interact to determine clinical outcomes.
Goals of Drug Administration
- Achieve systemic circulation
→ The drug must be absorbed into the bloodstream to reach its target tissue. - Ensure active form (free drug)
→ Only free (unbound) drug molecules can interact with receptors or enzymes to exert therapeutic effects.
Routes of Administration
The method chosen for drug delivery depends on:
- Desired onset and duration of action
- Drug solubility, stability, and pH compatibility
- First-pass metabolism and bioactivation requirements (e.g. prodrugs)
Table: Common Routes of Drug Administration
| Route | Advantages | Disadvantages |
|---|---|---|
| Oral (PO) | Convenient, large surface area, low cost | Incomplete absorption, first-pass metabolism, GI irritation |
| Buccal/Sublingual (SL) | Rapid onset, no first-pass effect | Short duration, requires lipid-soluble drug |
| Rectal (PR) | Useful if NPO/unconscious, minimal first-pass effect | Inconvenient, erratic absorption |
| Intravenous (IV) | Complete bioavailability, titratable, no first-pass | Invasive, expensive, irreversible once given |
| Intramuscular (IM) | Good for depot injections, moderate onset | Painful, risk of hematoma |
| Subcutaneous (SC) | Suitable for small, non-irritating doses | Smaller volumes, slower onset than IM |
| Intrathecal | Direct CNS access, bypasses BBB | High infection risk |
| Inhalation | Immediate lung action, no first-pass | Requires gas/vapour delivery system |
| Topical | Localised effect, easy to apply | Limited systemic use, local irritation |
| Transdermal | Sustained systemic effect, bypasses GI/liver | Delayed onset, not ideal for hydrophilic drugs |
| Other (e.g. intra-articular, intraperitoneal) | Local effect | Risk of infection, technical skill required |
Drug Distribution and Tissue Reservoirs
- Free drug in circulation is pharmacologically active.
- However, some drug binds to tissue reservoirs or plasma proteins (e.g. albumin).
- Bound ↔ Free equilibrium: as free drug is metabolised, more is released from storage.
This affects:
- Duration of action
- Drug availability
- Therapeutic window
Target of Action
- Consider where the drug needs to act:
- Does it require CNS access?
- Is it acting locally or systemically?
- Ask: Can free drug in the blood reach its target receptor/enzyme/cell?
Biotransformation (Drug Metabolism)
Most metabolism occurs in the liver, involving two main processes:
1. Bioactivation
- Inactive prodrug → Active metabolite
E.g. codeine → morphine
2. Bioinactivation
- Active drug → Inactive metabolite (usually water-soluble)
3. Detoxification
- Toxic substances → Non-toxic metabolites
4. Conjugation
- Enhances water solubility → Aids renal excretion
Key Consideration:
- Does the drug pass through the liver before reaching its target?
→ Oral = Yes (first-pass metabolism)
→ IV = No (enters systemic circulation directly)
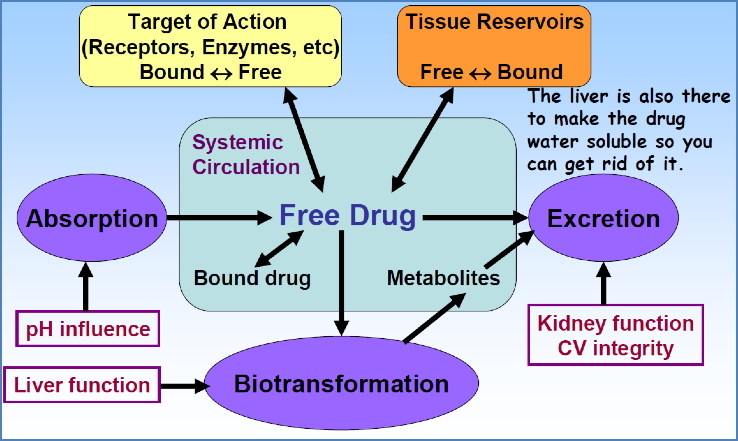
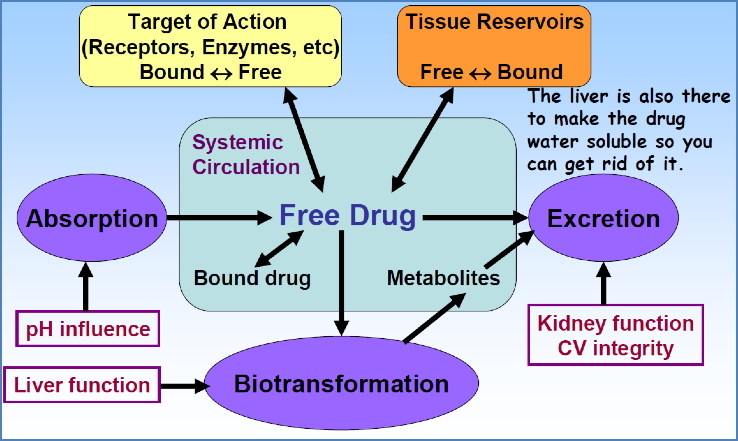
Excretion
- Most drugs are excreted by the kidneys
- Must be water-soluble to be efficiently eliminated in urine
- Lipid-soluble drugs may require hepatic conversion first
Pharmacokinetics vs Pharmacodynamics
| Concept | Definition |
|---|---|
| Pharmacokinetics | What the body does to the drug: Absorption, distribution, metabolism, excretion |
| Pharmacodynamics | What the drug does to the body: Binding to targets, causing effects |
Both influence whether a drug will reach its target and produce a therapeutic effect.
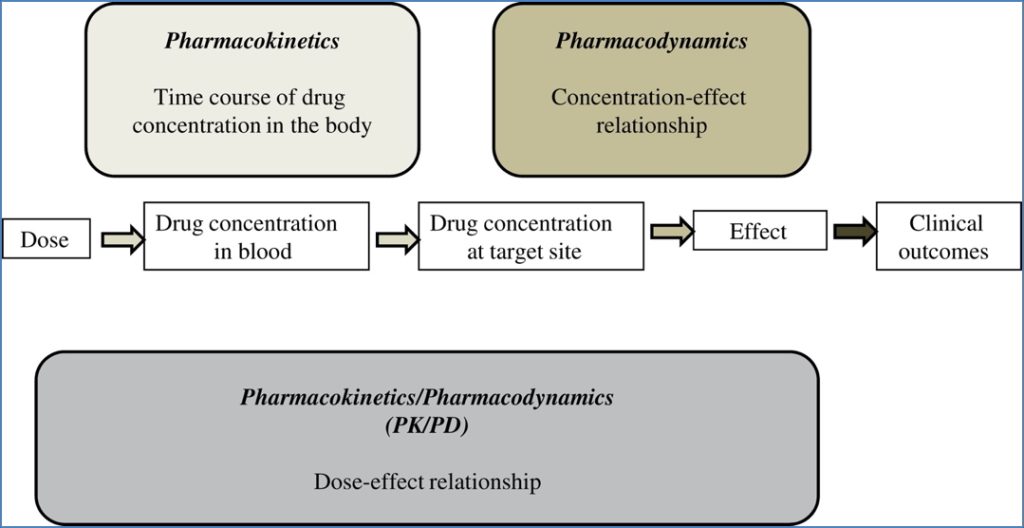
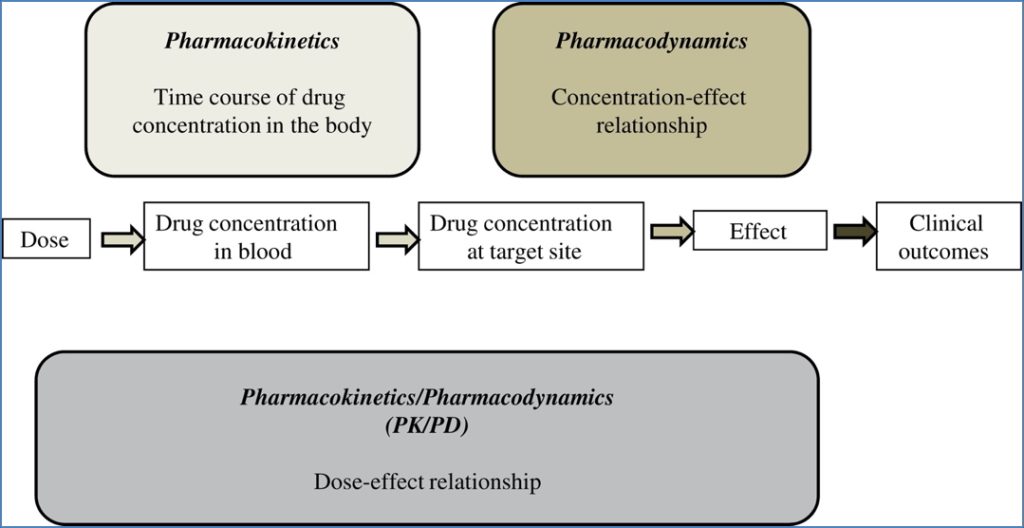
Summary – Drug Administration
Drug administration plays a pivotal role in determining whether a medication will reach its target, remain in active form, and be safely eliminated. Understanding routes, distribution, metabolism, and the interaction between pharmacokinetics and pharmacodynamics is essential for optimal therapeutic effect. For a broader context, see our Pharmacology & Toxicology Overview page.