Table of Contents
Overview – Pregnancy
Pregnancy is a dynamic physiological process initiated by fertilisation, followed by implantation, embryonic development, and placental formation. This article provides a comprehensive overview of early pregnancy — from clinical signs and hormonal markers to blastocyst implantation and placentation. Understanding this timeline is crucial for interpreting antenatal tests, managing early pregnancy issues, and preparing for OSCE stations.
Aetiology
- Unprotected sexual intercourse
- In vitro fertilisation (IVF)
- Artificial insemination (AI)
Clinical Features
Symptoms
- Amenorrhoea
- Nausea and vomiting
- Heartburn or reflux
- Breast tenderness
- Urinary frequency
- Constipation
- Fatigue
Signs
- Softening of the cervix (by 4–6 weeks)
- Chadwick’s sign: Bluish vaginal mucosa due to vascular engorgement
- Uterine enlargement
- Breast enlargement and areolar darkening
Diagnosis of Pregnancy
β-hCG Testing
- Serum: Positive ~9 days post-conception
- Urine: Positive ~28 days post-conception
Ultrasound Findings
- Transvaginal:
- 5 weeks: Gestational sac visible
- 6 weeks: Foetal pole visible
- 7–8 weeks: Foetal heartbeat detectable
- Transabdominal:
- 6 weeks: Detectable intrauterine pregnancy
Physiological Amenorrhoea in Pregnancy
- Trophoblasts secrete β-hCG, maintaining the corpus luteum → continuous oestrogen and progesterone secretion → prevents menstruation.
- Trophoblasts → Chorion → continues β-hCG production.
- Placenta takes over hormone production around the end of the first trimester.
Low β-hCG for gestational age may indicate ectopic pregnancy, miscarriage, or incorrect dating.


Fertilisation & Implantation
Fertilisation Window
- Oocyte: Viable up to 24 hrs post-ovulation.
- Sperm: Viable up to 48 hrs in female tract.
- Fertilisation typically occurs in the ampulla of the fallopian tube.
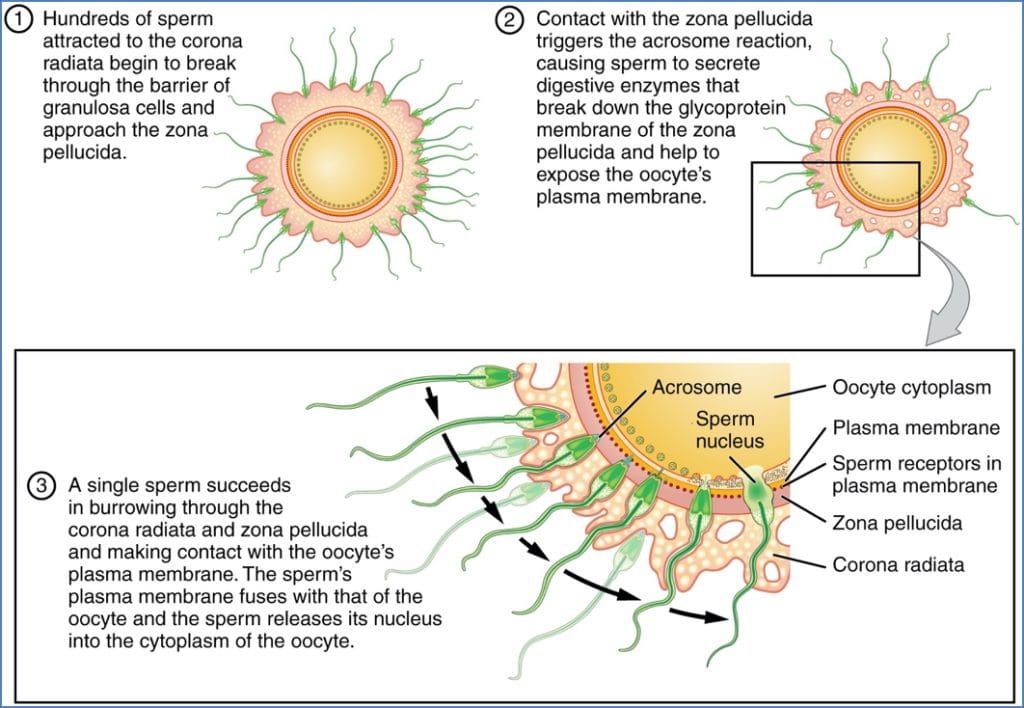
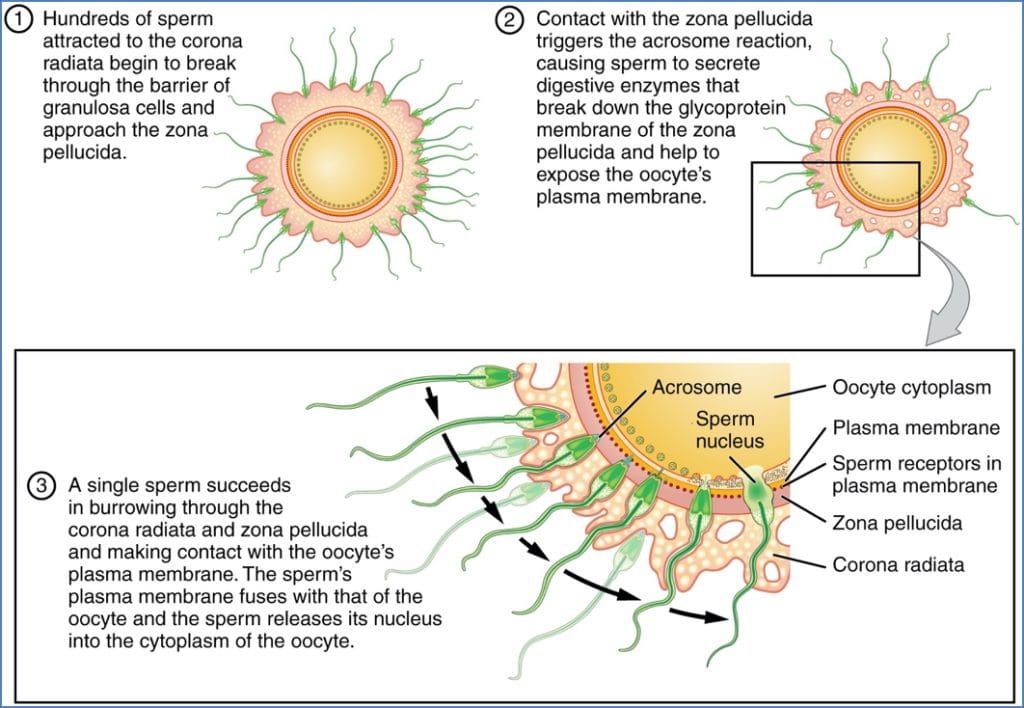
Sperm Capacitation & Penetration
- Sperm are capacitated by female tract secretions.
- Corona radiata penetrated by hyaluronidase.
- Zona pellucida digested via acrosomal enzymes (requires hundreds of sperm).
- One sperm fuses with oocyte membrane → triggers cortical reaction → prevents polyspermy.
- Secondary oocyte completes meiosis II → forms ovum + second polar body.
- Sperm loses tail and swells → male pronucleus.
- Male and female pronuclei fuse → zygote forms.
- Mitosis begins (cleavage).
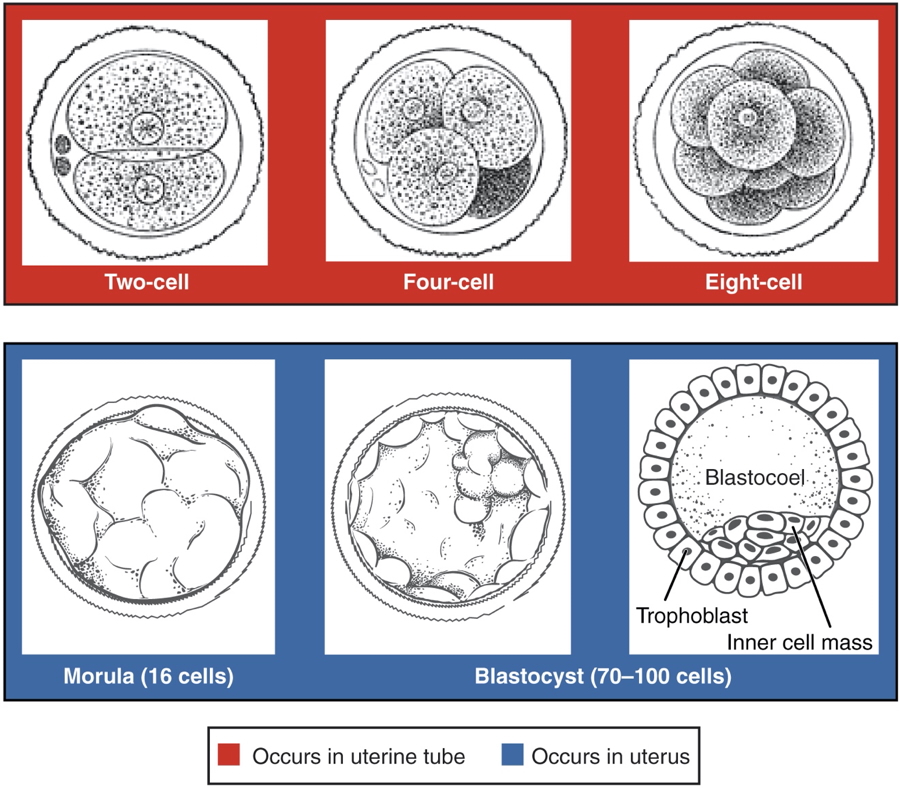
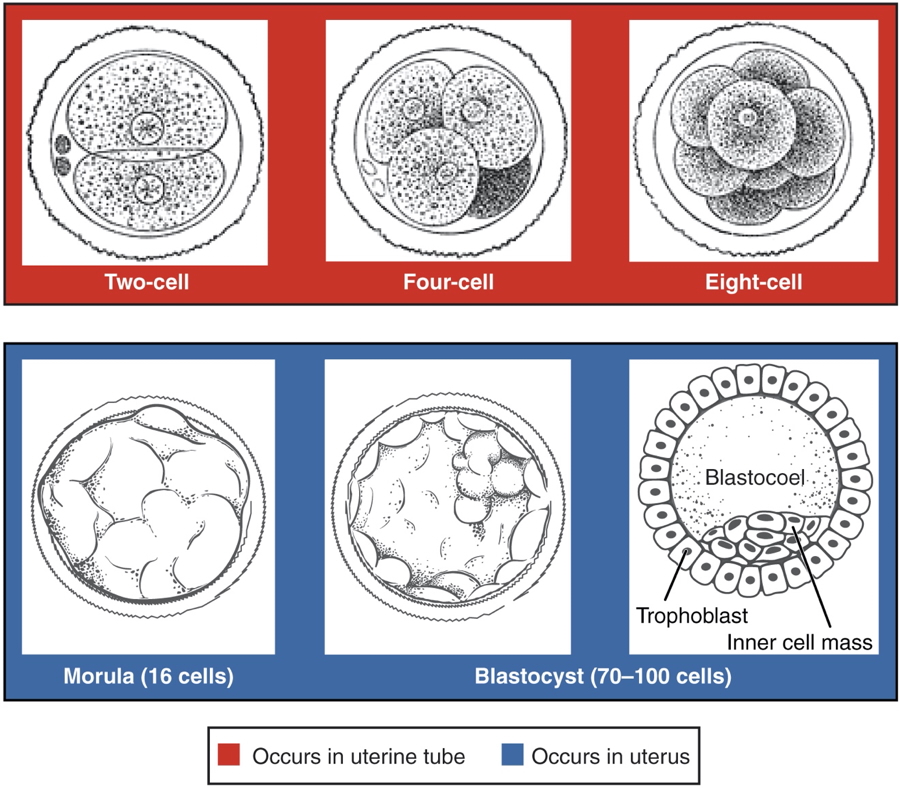
From Zygote to Blastocyst Implantation
Cleavage & Blastocyst Formation
- Zygote undergoes rapid mitosis → morula.
- Blastocyst forms as fluid accumulates inside morula.
- Zona pellucida degrades → blastocyst hatches.
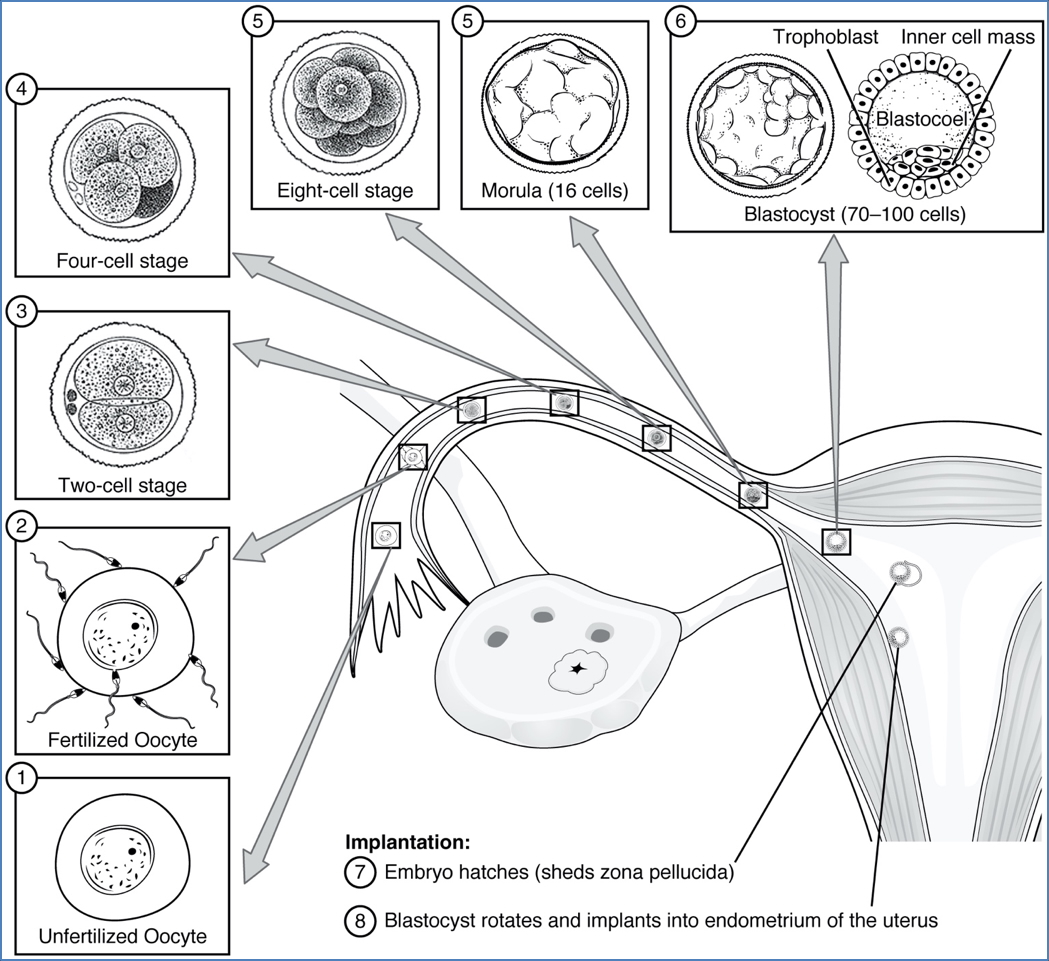
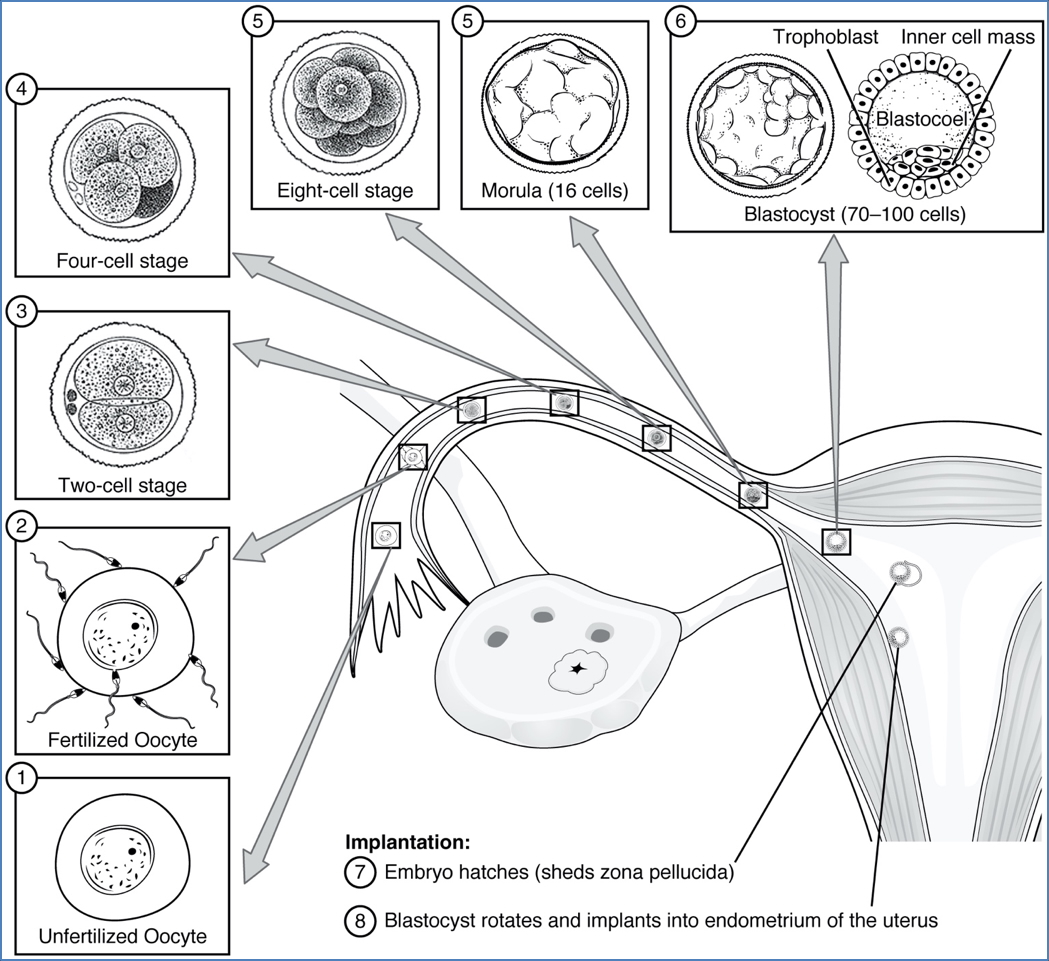
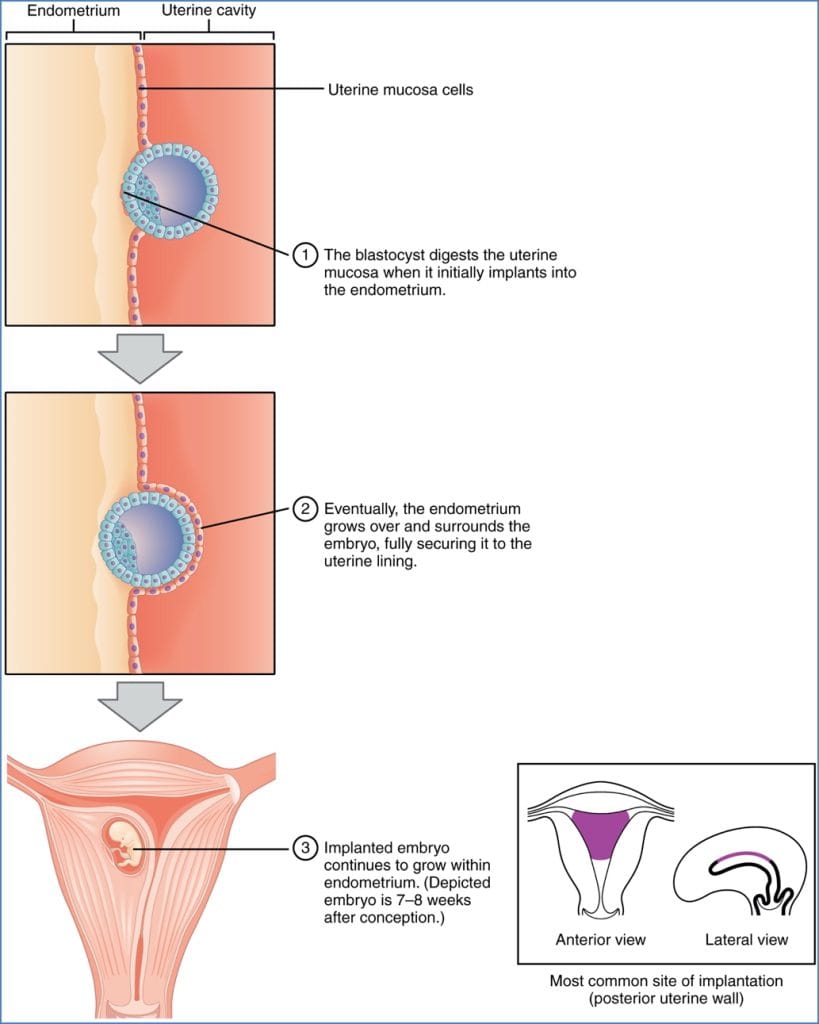
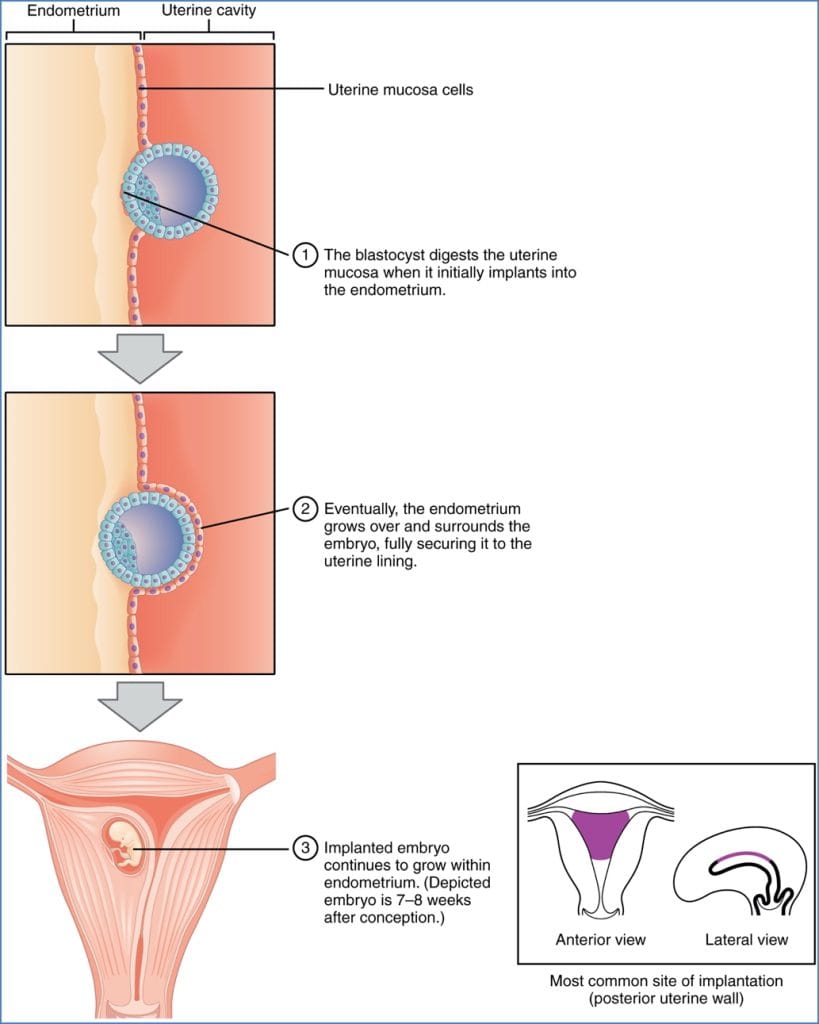
Implantation (6–12 Days Post-Ovulation)
- Requires receptive endometrium (secretory phase).
- Trophoblasts bind to endometrial matrix, may “float” and reattach if initial contact fails.
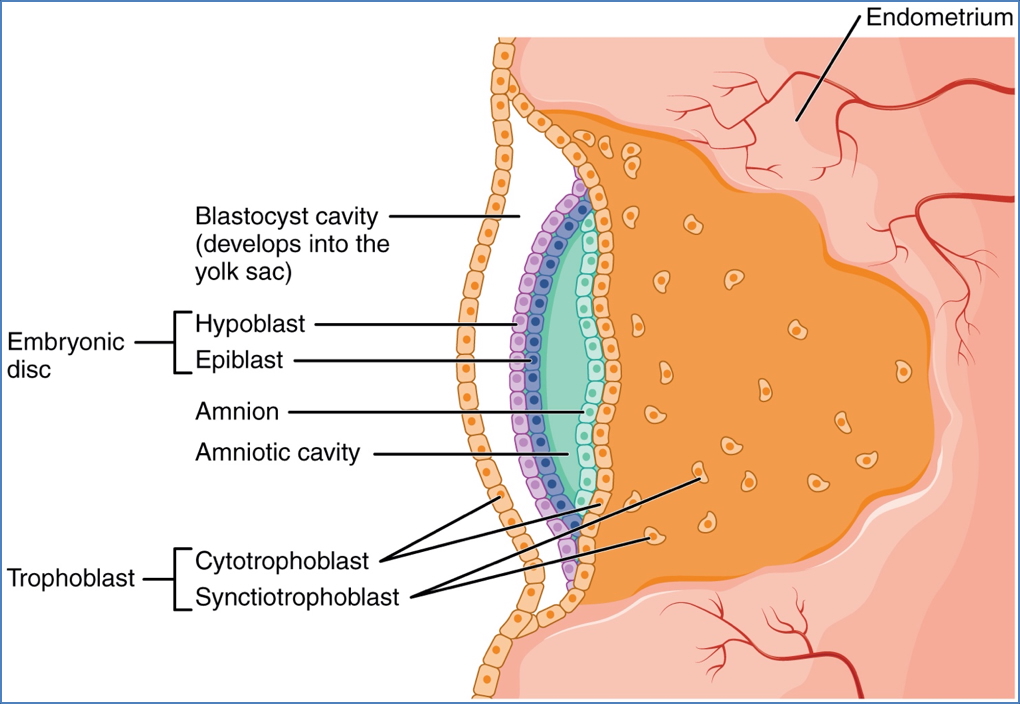
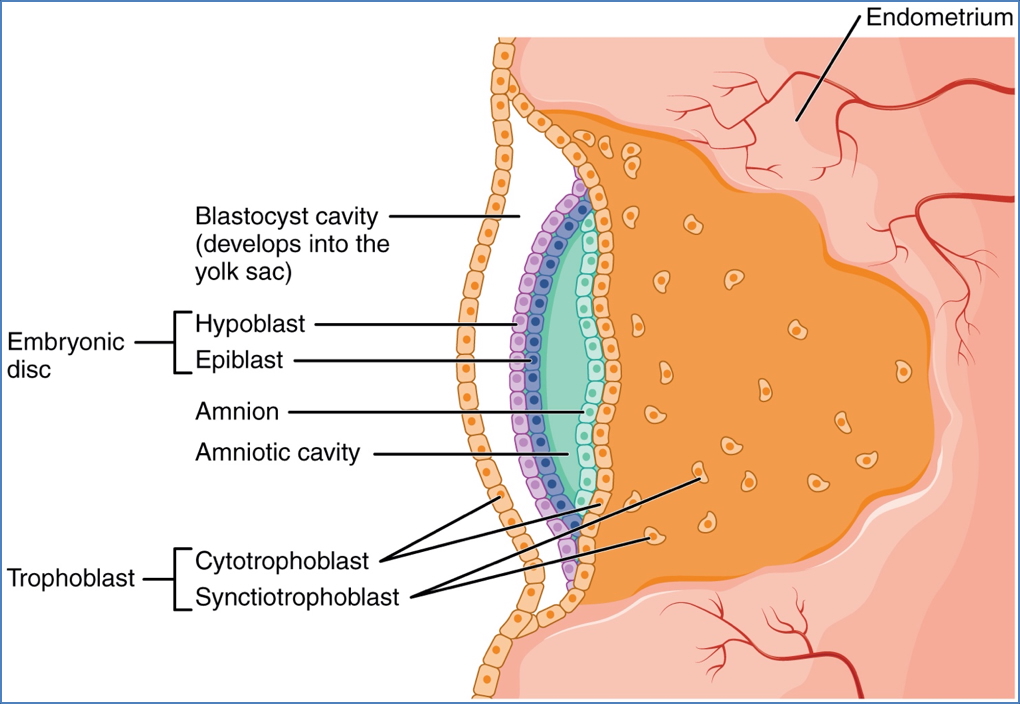
- Two trophoblast layers form:
- Cytotrophoblast (inner)
- Syncytiotrophoblast (outer, invasive)
- Syncytiotrophoblast digests uterine tissue → embryo gains access to maternal nutrients.
- Implantation completes by ~Day 12 → trophoblasts secrete β-hCG to maintain corpus luteum.
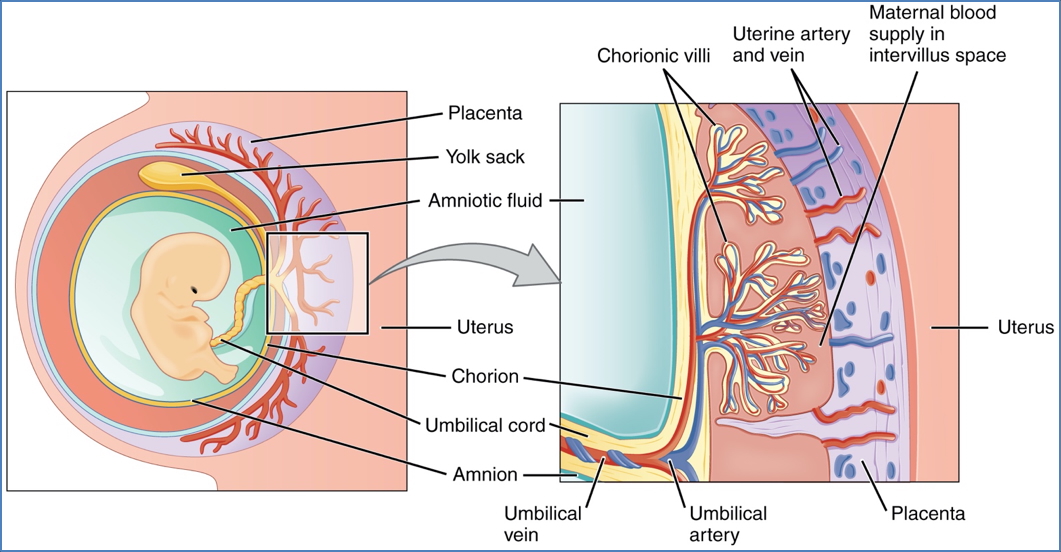
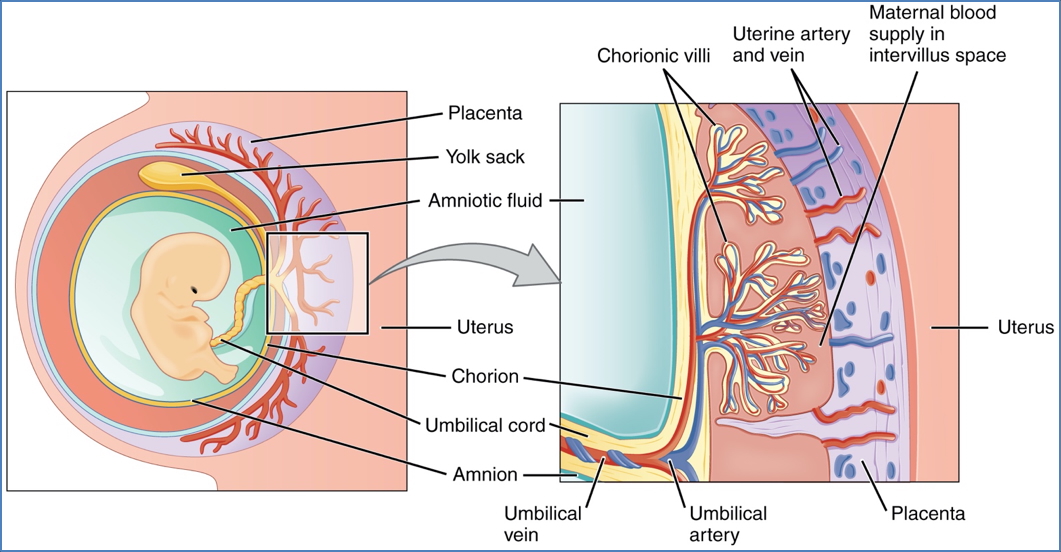
Placentation
Chorion Formation
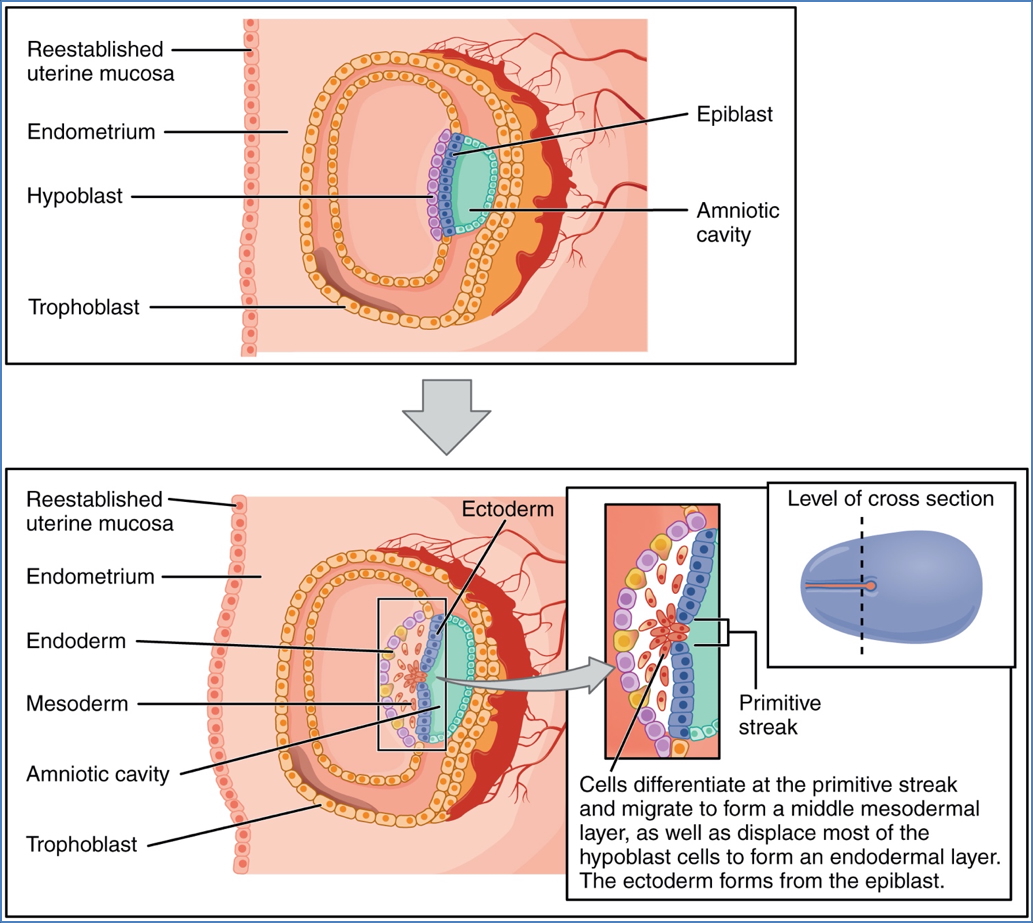
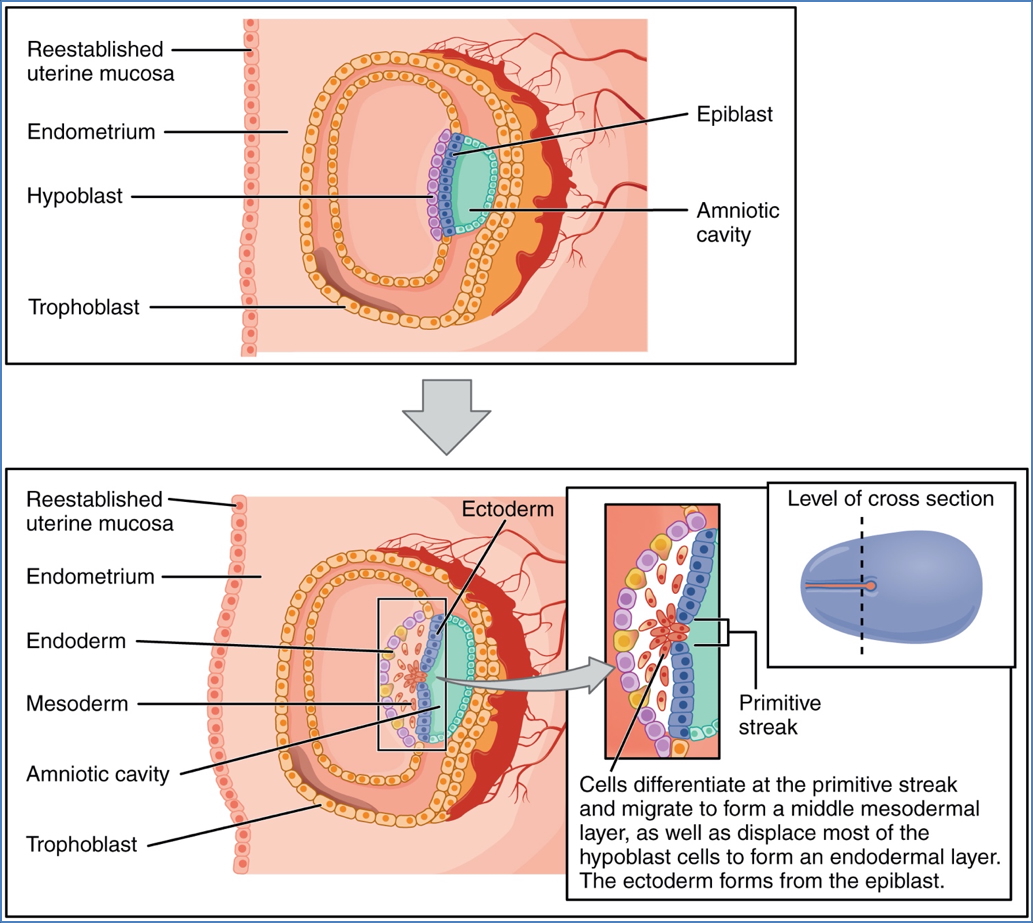
- Extraembryonic mesoderm + cytotrophoblast → chorion.
- Chorionic villi develop and invade maternal blood pools (lacunae).
Decidualisation of Endometrium
- Decidua basalis: Site of placental formation (maternal side).
- Decidua capsularis: Surrounds embryo; eventually degenerates as uterus expands.
Placental Functions
- Nutritional: Glucose, amino acids, fatty acids
- Respiratory: Oxygen and carbon dioxide exchange
- Excretory: Waste removal
- Endocrine: Secretes hCG, progesterone, oestrogen


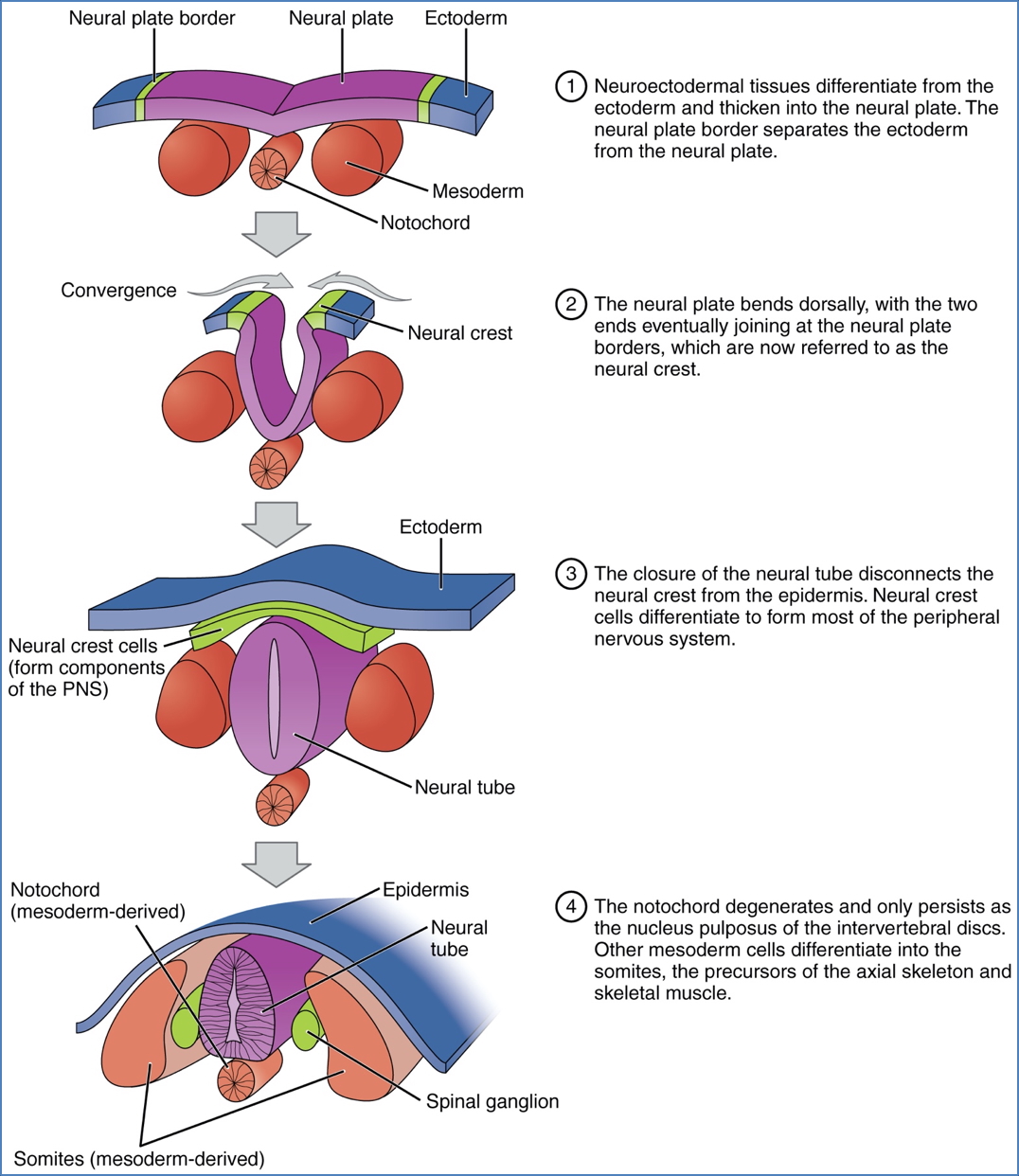
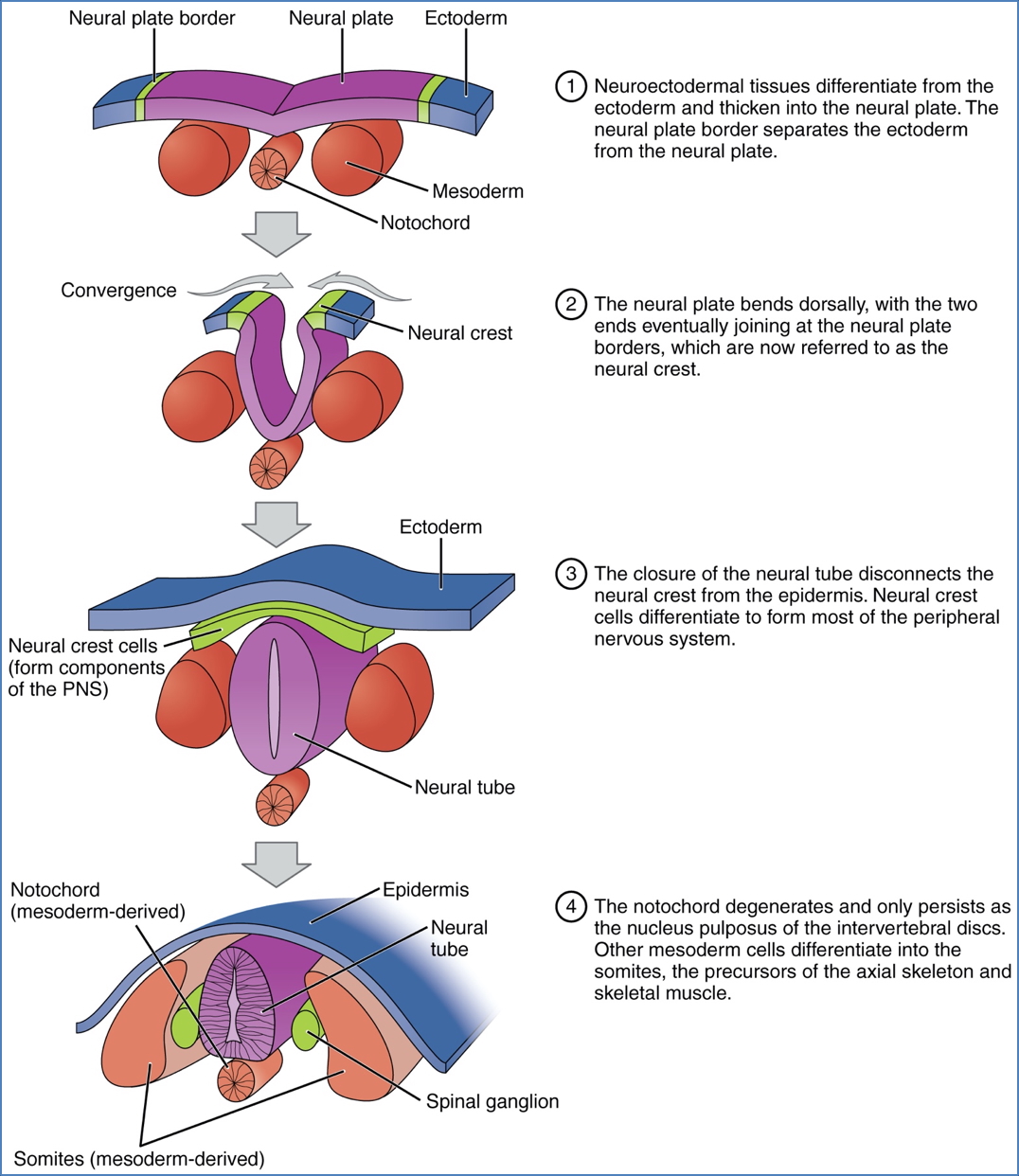
Embryonic Development Overview
Germ Layer Formation
- Ectoderm: Skin, nervous system, amnion
- Mesoderm: Heart, vessels, muscle, bone, connective tissue
- Endoderm: GI, respiratory, urinary epithelium, yolk sac
By 8 weeks, all organ systems have begun to form.


Summary – Pregnancy
Pregnancy begins with fertilisation and proceeds through cleavage, implantation, placentation, and embryonic development. β-hCG plays a critical role in maintaining early gestation and signals pregnancy on clinical testing. Understanding these milestones is vital for managing antenatal care. For a broader context, see our Obstetrics Overview page.