Table of Contents
Overview – Neonatal Jaundice & Kernicterus
Neonatal jaundice is a common condition occurring in newborns due to the accumulation of unconjugated bilirubin, resulting in yellowing of the skin and sclera. While usually benign and self-limiting, extremely elevated bilirubin levels can lead to kernicterus, a form of bilirubin-induced brain damage. Prompt recognition and treatment are critical to avoid irreversible complications, including seizures, hearing loss, and intellectual disability.
Definition
- Neonatal Jaundice: Yellowing of the skin and sclera in newborns caused by hyperbilirubinemia, particularly unconjugated bilirubin.
- Kernicterus: A severe neurological complication of extreme hyperbilirubinemia, characterised by deposition of bilirubin in the brain tissue—especially in the basal ganglia and thalamus.
Aetiology
- Increased Bilirubin Production:
- Due to increased breakdown of foetal red blood cells, which have a shorter lifespan.
- Reduced Hepatic Clearance:
- Immature neonatal liver lacks sufficient glucuronyl transferase activity for conjugation of bilirubin.
Pathophysiology
- Neonates exhibit both an increased rate of red cell turnover and an immature liver enzyme system.
- This results in a transient rise in unconjugated bilirubin.
- If levels exceed the albumin-binding capacity, free bilirubin crosses the blood-brain barrier.
- Deposition occurs in deep brain nuclei → Kernicterus
- Can result in permanent neurological damage, especially to auditory and motor centres.
Morphology
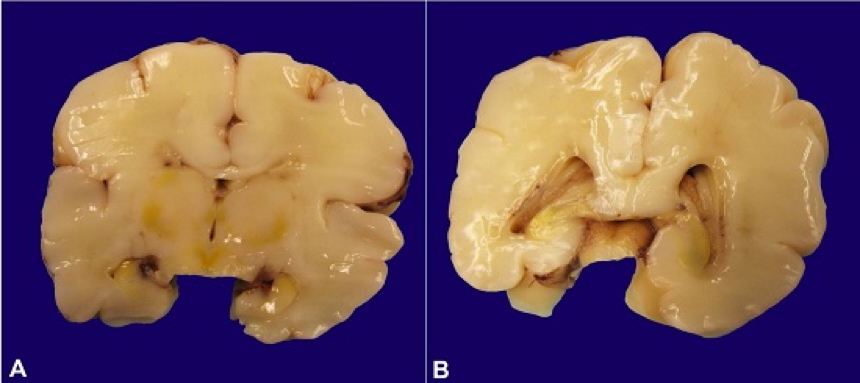
- Macroscopic Findings:
- Yellow discoloration of the basal ganglia, thalamus, cerebellum, tegmentum, and ventricular floor
- The term “Kernicterus” comes from “kern” (nucleus) and “icterus” (jaundice) = “yellow nuclei”
Clinical Features
- Signs of Jaundice:
- Yellowing of the skin and eyes within the first week of life
- Neurological Signs (suggestive of Kernicterus):
- Poor feeding
- Hypersomnolence
- Absent Moro (startle) reflex
- Bulging fontanel
- Hypotonia → later spasticity

Investigations
- Serum bilirubin levels (total and conjugated/unconjugated)
- Blood group compatibility and Coombs test (to rule out haemolysis)
- Sepsis screen if infection is suspected
Management
- Phototherapy:
- First-line for unconjugated hyperbilirubinemia
- Converts bilirubin into water-soluble isomers excretable in urine and bile
- Exchange Transfusion:
- Indicated in severe cases or signs of bilirubin encephalopathy
- Replaces the baby’s blood to reduce bilirubin and address haemolysis
- Vitamin K:
- Not directly treating jaundice, but important in all neonates to prevent haemorrhagic disease of the newborn
Complications
- Auditory:
- High-frequency hearing loss
- Neurological:
- Cerebral palsy
- Developmental delay
- Seizures
- Intellectual disability
- Motor and Speech:
- Dysarthria and delayed milestones
Summary – Neonatal Jaundice & Kernicterus
Neonatal jaundice results from increased bilirubin production and reduced hepatic clearance in newborns. Although typically benign, untreated severe hyperbilirubinemia can progress to kernicterus, causing irreversible neurological injury. Early signs include poor feeding, lethargy, and a bulging fontanel. Prompt treatment with phototherapy or exchange transfusion is essential. For a broader context, see our Obstetrics Overview page.