Table of Contents
Overview – Antenatal Care
Antenatal care is the essential foundation of maternal and fetal wellbeing during pregnancy. It begins even before conception and includes screening, education, supplementation, and timely interventions to prevent complications. This page outlines high-yield knowledge for final-year medical students, covering pre-conception counselling, safe medications, immunisation protocols, lifestyle guidance, and the key components of the first prenatal visit.
Pre-Conception Counselling
Folate Supplementation
- Reduces the risk of neural tube defects by up to 70%.
- Begin 8–12 weeks pre-conception and continue through the first 3 months of pregnancy.
- Dosage:
- 0.4–1 mg daily for low-risk women.
- 5 mg daily for higher-risk groups (e.g. previous NTDs, anticonvulsants, diabetes, obesity).

Additional Supplements
- Iron supplementation
- Prenatal multivitamins
Medication Precautions in Pregnancy
Absolute Contraindications
- ACE inhibitors: Fetal renal anomalies, IUGR, oligohydramnios.
- Tetracyclines: Dental staining, impaired bone growth.
- Retinoids (e.g. isotretinoin): CNS, craniofacial, cardiac, thymic anomalies.
- Misoprostol: Mobius syndrome, spontaneous abortion, preterm labour.
Relative Contraindications
- Phenytoin: Fetal hydantoin syndrome.
- Valproate / Carbamazepine: Neural tube defects (1–2% risk).
- Lithium: Ebstein’s anomaly, goitre, hyponatraemia.
- Warfarin: Abortion, IUGR, fetal warfarin syndrome.
- Erythromycin: Maternal acute fatty liver.
- Sulphonamides: Anti-folate, risk of kernicterus.
- Chloramphenicol: Grey baby syndrome.
Important Immunisations
Pre-Conception (Live Vaccines)
- Avoid live vaccines during pregnancy – administer before conception if non-immune:
Safe During Pregnancy
- Tetanus
- Diphtheria
- Pertussis
- Influenza (recommended)
- Hepatitis B
Postpartum Recommendations
- Rubella for all non-immune mothers.
- Hepatitis B vaccine for all neonates (within 12 hours if maternal status is unknown or positive).
- Other routine immunisations may resume after delivery.
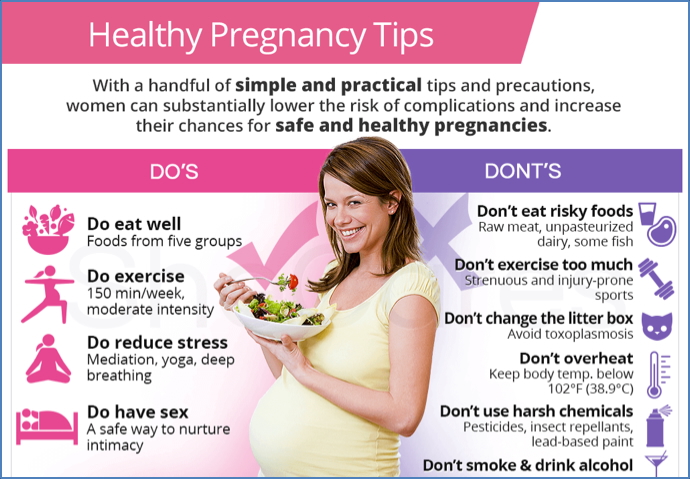
Optimising Health During Pregnancy
- Exercise: Regular moderate activity (e.g. walking) maintains strength, mood, and healthy weight.
- Nutrition:
- Balanced diet with key nutrients.
- Avoid high-risk foods: soft cheeses, raw fish.
- Limit caffeine.
- Substance Avoidance:
- No smoking, alcohol, or recreational drugs.
- Review all prescription medications with a healthcare provider.
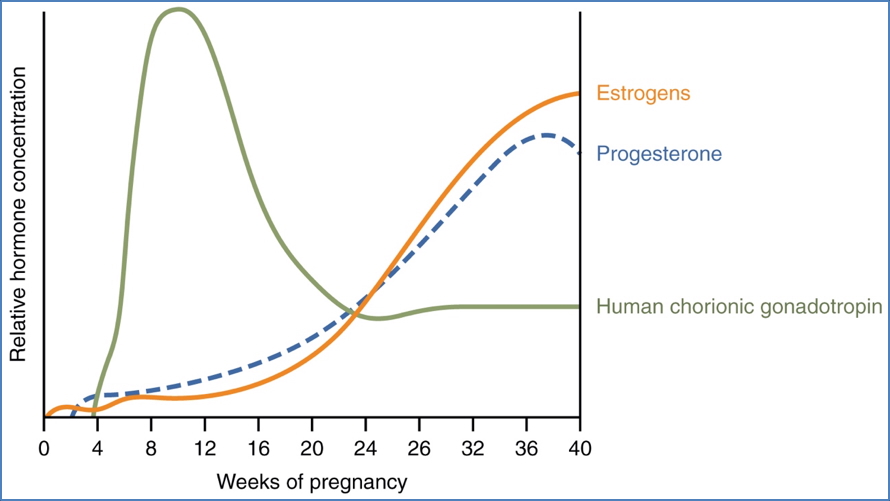
Pregnancy Hormones
- Oestrogen rises between 6–12 weeks gestation:
- Prevents menstruation.
- Can cause morning sickness and mood swings.
- Morning sickness often resolves by 3–4 months, but may persist throughout pregnancy.
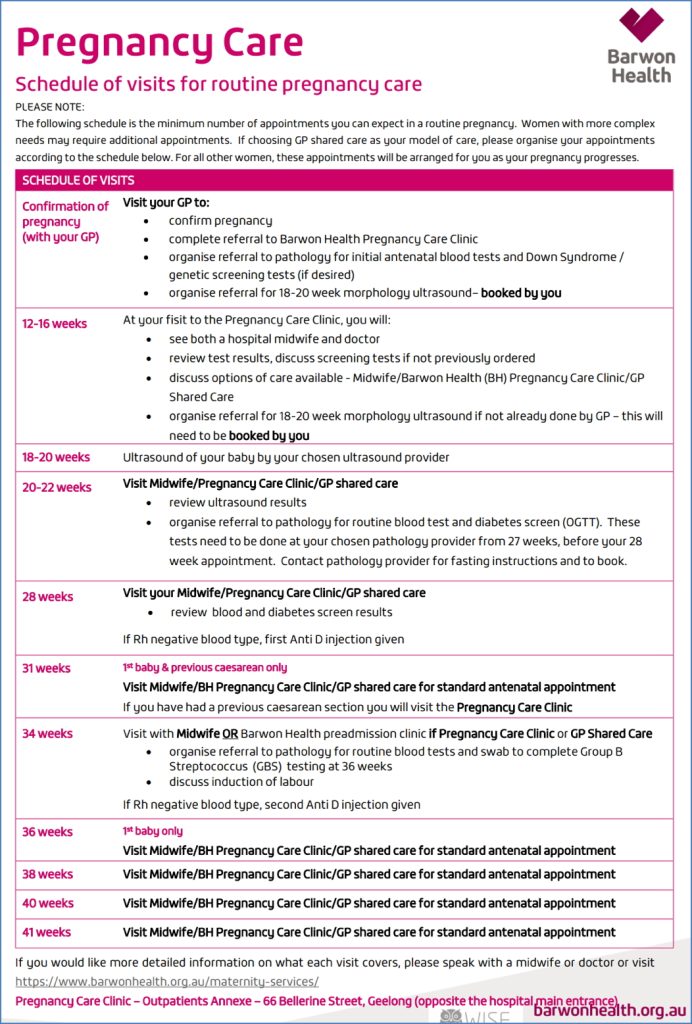
The Initial Prenatal Visit
Timing
- Usually between 8–12 weeks gestation (based on last menstrual period).
- Consider earlier review if:
- Bleeding
- Hyperemesis
- Teenage pregnancy
- Maternal age >35
History Taking
- Medical and surgical history
- Gynaecological and obstetric history
- Medications and allergies
- Family/genetic history
- Social history (smoking, alcohol, drug use)
Physical Examination
- General examination
- Baseline BP, weight
- Pelvic exam (if indicated)
Investigations
- Blood tests:
- Full blood count
- Blood group and Rhesus (Rh) status
- Antibody screen
- Urinalysis: Bacteriuria and proteinuria
- STI screen: Gonorrhoea and chlamydia PCR
- Pap smear: If due and appropriate
Pregnancy Dating
- Based on LMP or by dating ultrasound (ideally at ~12 weeks gestation).
Summary – Antenatal Care
Antenatal care involves proactive maternal and fetal health management beginning before conception. Key components include supplementation, medication review, safe immunisation, lifestyle modification, and structured assessments during early pregnancy. For a broader context, see our Obstetrics Overview page.