Table of Contents
Overview – Pulmonary Tuberculosis
Pulmonary tuberculosis is a chronic infectious disease caused by Mycobacterium tuberculosis, primarily affecting the lungs and spread through airborne droplets. It is a major global health concern, particularly in low-resource settings, and can progress from asymptomatic latent infection to severe pulmonary damage or systemic spread. Understanding its clinical presentation, diagnostic approach, and management is essential for all medical students preparing for finals and clinical practice.
Definition
Pulmonary tuberculosis (TB) is a granulomatous infection of the lungs caused by the inhalation of Mycobacterium tuberculosis, an acid-fast bacillus. It may remain latent or progress to active disease, potentially spreading throughout the body (miliary TB).
Aetiology
- Causative Organism:Mycobacterium tuberculosis
- Acid-fast bacillus
- Transmitted via airborne droplets from an infected individual
Pathophysiology
Primary Pulmonary Tuberculosis
- Bacilli are inhaled → reach alveoli
- Phagocytosed by alveolar macrophages
- Multiply intracellularly → localised infection
- ~3 weeks later: adaptive immunity kicks in
- CD4+ Th1 cells → secrete interferon-gamma (IFN-γ)
- Activates macrophages → formation of caseating granulomas
Caseating Granulomas
- Central area of caseous necrosis (“cheese-like” appearance)
- Surrounded by epithelioid cells, multinucleated Langerhans giant cells, lymphocytes, and fibroblasts
Ghon Focus and Ghon Complex
- Ghon focus: 1–1.5 cm area of gray-white inflammation with caseous necrosis
- Ghon complex: Ghon focus + involvement of regional hilar lymph nodes
Miliary Tuberculosis
- Bacteria disseminate via lymphatics and blood
- Multiple lesions (“millet seed” appearance) form in lungs and other organs
- May erode into lung parenchyma → pleural effusion, haemoptysis, empyema
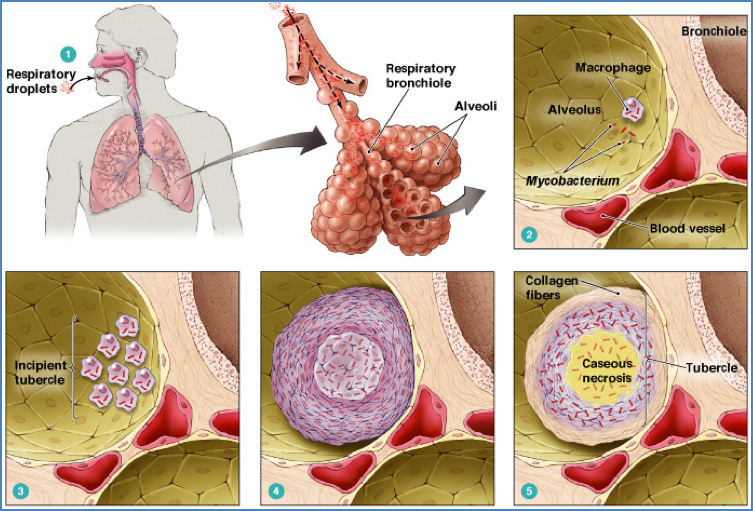
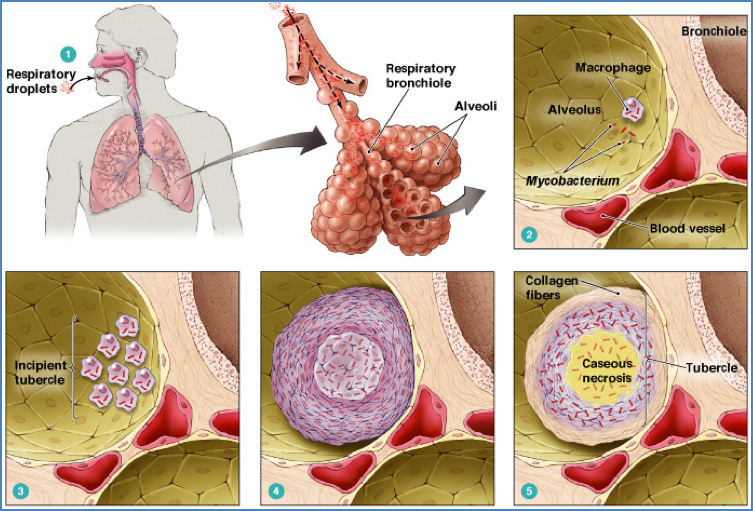
Morphology
- Predominantly affects upper lobes of the lungs
- Caseating granulomas
- Central necrosis with a rim of inflammatory cells
- May cavitate, fibrose, or calcify
- Ghon complex may be visible on imaging
- Miliary lesions are small, scattered nodules throughout the lung fields


Clinical Features
- May be asymptomatic in latent TB
- Typical symptoms (active TB):
- Chronic productive cough
- Fever and night sweats
- Weight loss
- Pleuritic chest pain
- Haemoptysis (if cavitation or vascular erosion present)
- Miliary TB symptoms:
- Respiratory failure
- Multisystem involvement depending on seeding
Investigations
Mantoux (Tuberculin) Test
- Intradermal injection of purified protein derivative (PPD)
- Delayed hypersensitivity reaction
- Becomes positive 2–4 weeks post-exposure
- Remains positive for life after infection
- Indicates T-cell sensitisation, not necessarily active disease


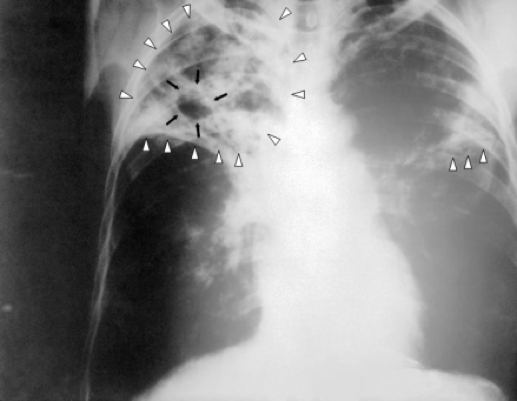
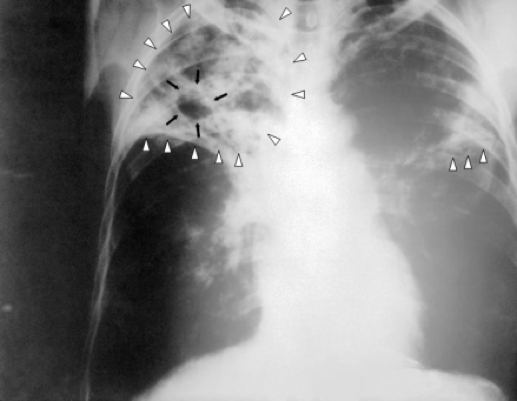
Imaging
- Chest X-ray (CXR):
- Upper lobe consolidation
- Ghon focus/complex
- Cavitary lesions (reactivation TB)
- Miliary pattern (in disseminated disease)
Microbiological Tests
- Sputum smear microscopy:
- Acid-fast bacilli (AFB)
- Culture & sensitivity testing:
- Takes several weeks but confirms diagnosis and detects drug resistance
- Polymerase chain reaction (PCR):
- Rapid and highly sensitive
Management
- Combination antibiotic therapy (usually for 6 months or longer):
- Rifampicin
- Isoniazid
- Pyrazinamide
- Ethambutol
- Monitor for adherence, hepatotoxicity, and resistance
- Longer courses required for drug-resistant TB or extrapulmonary TB
Complications
- Pulmonary complications:
- Cavitary destruction
- Haemoptysis, pleural effusion, pneumothorax
- Systemic complications (miliary TB):
- Spread to CNS, bones, kidneys, liver
- TB meningitis, Pott’s disease, renal TB
- Treatment-related:
- Hepatotoxicity
- Peripheral neuropathy (especially with isoniazid)
Differential Diagnosis
- Pneumonia
- Lung abscess
- Bronchogenic carcinoma
- Fungal infections (e.g. histoplasmosis)
- Sarcoidosis
- Lymphoma
Summary – Pulmonary Tuberculosis
Pulmonary tuberculosis is a chronic infectious condition caused by Mycobacterium tuberculosis, typically affecting the upper lobes of the lungs. It can be latent or progress to active disease, characterised by chronic cough, fever, weight loss, and night sweats. Classic histology reveals caseating granulomas and Ghon complexes. Diagnosis involves the Mantoux test, sputum microscopy, and imaging. Treatment requires long-term combination antibiotics. For a broader context, see our Microbiology & Public Health Overview page.