Table of Contents
Overview – Transplant Immunology
Transplant immunology is the study of the immune system’s response to transplanted organs and tissues. Understanding the immunological principles that govern graft survival and rejection is essential in clinical medicine, especially for managing organ and bone marrow transplantation. Immune rejection remains a major challenge despite modern advances in matching and immunosuppressive therapy.
Definition
Transplant immunology is the branch of immunology concerned with the immune response to transplanted tissues and organs, including the mechanisms of graft rejection and the strategies used to prevent it.
Types of Transplant Grafts
- Autograft – Transplant from self to self → No rejection risk
- Isograft – From identical twin to twin → Minimal rejection risk
- Allograft – From one human to another → Rejection possible
- Xenograft – From animal to human → High rejection risk
Principles of Transplant Immunology
Alloantigens
- Alloantigens are antigens that differ among individuals of the same species.
- Major Histocompatibility Complex (MHC) is the most immunogenic alloantigen.
- Minor histocompatibility antigens also contribute to rejection despite MHC matching.
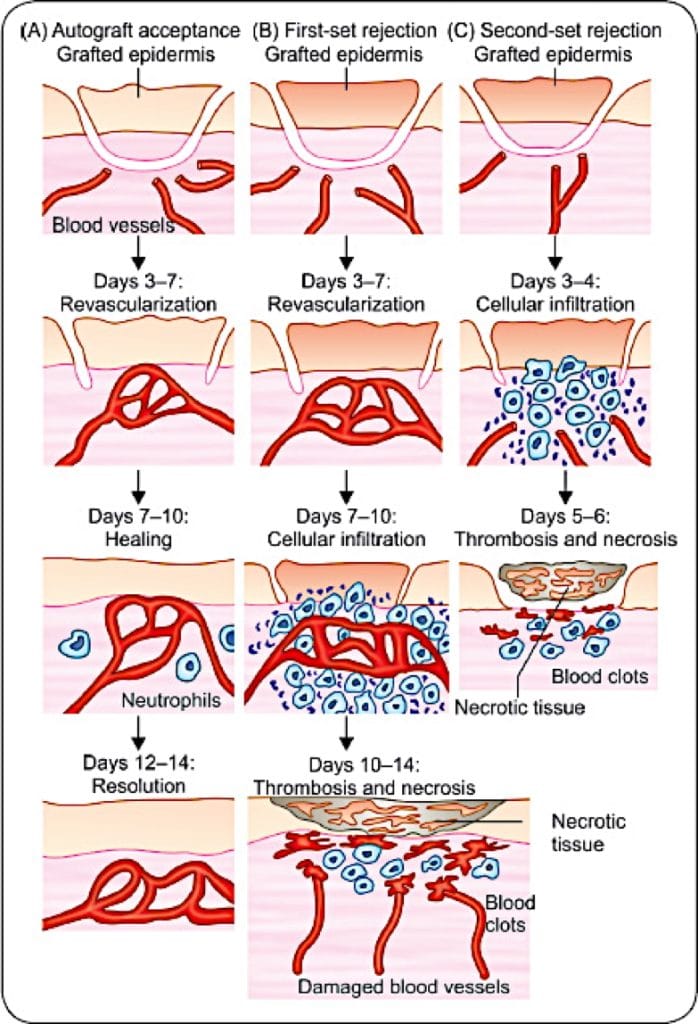
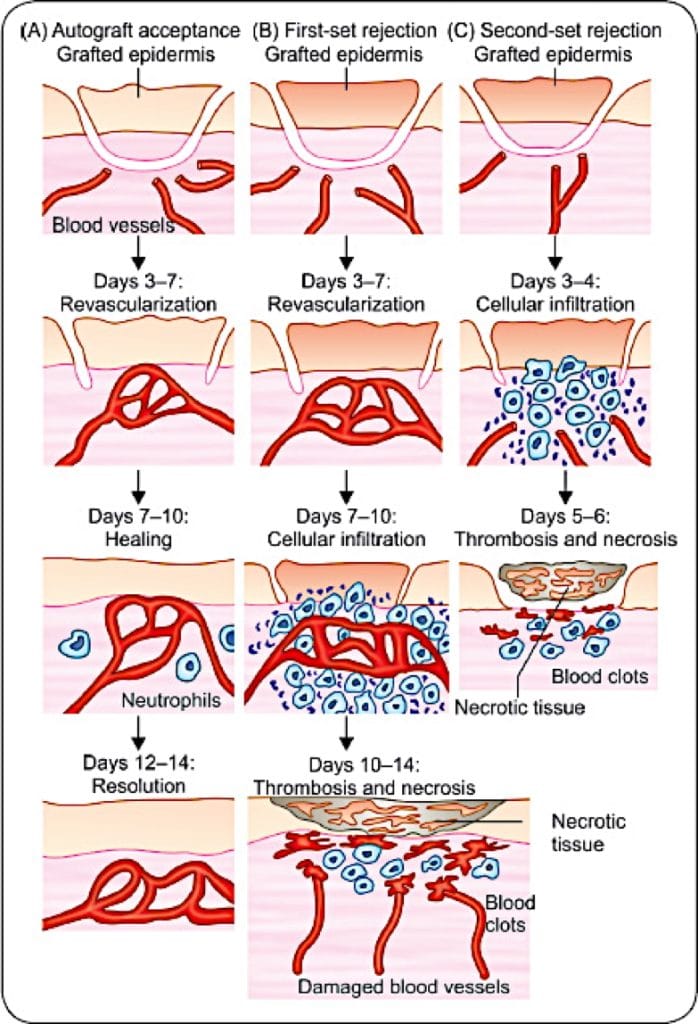
1st-Set vs 2nd-Set Rejection
- 1st-Set Rejection:
- Graft given to naïve individual → Rejected after sensitisation
- 2nd-Set Rejection:
- Graft from same donor given to sensitised host → Rapid rejection
- Lymphocyte transfer from sensitised to naïve host can confer 2nd-set rejection
Alloimmune Response Pathways
Direct Allorecognition
- Donor antigen-presenting cells (APCs) in graft migrate to host lymph nodes
- Present donor MHC to host T-cells → Activate alloreactive T-cells
- Responsible mainly for acute rejection
Indirect Allorecognition
- Host APCs process donor antigens and present on self-MHC
- Activates host T-cells that attack the graft
Afferent vs Efferent Arms
- Afferent: Sensitisation (Direct or Indirect Allorecognition)
- Efferent: Effector lymphocytes mount immune attack
Role of T-Cells
- CD8+ T-cells cause cytotoxic graft destruction
- CD4+ T-cells activate:
- Macrophages → Tissue injury
- B-cells → Alloantibody production
Clinical Transplantation
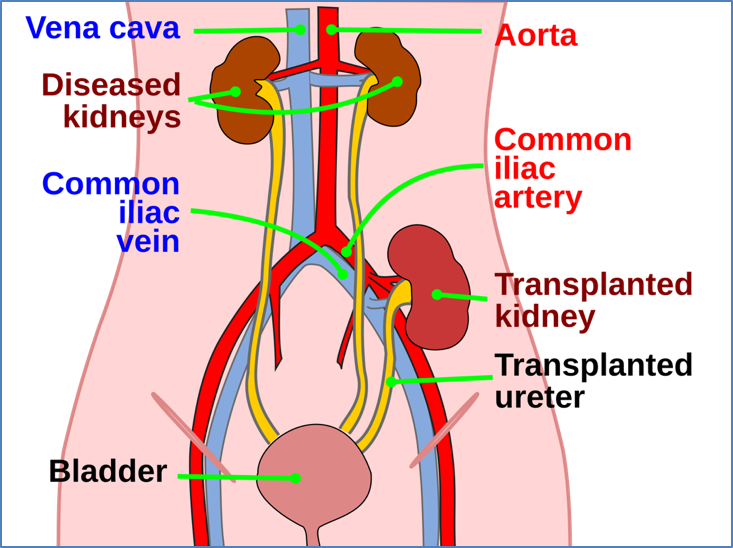
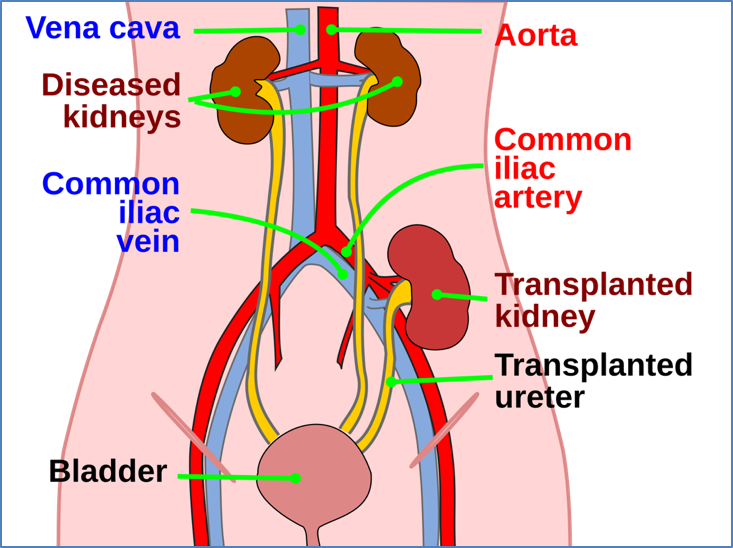
Kidney Transplant
- Indication: End-stage renal failure
- Essential Matching Criteria:
- ABO compatibility
- Negative T-cell crossmatch
- No prior anti-donor HLA antibodies
- Other Considerations: HLA matching, viral status, transfusion history
- Complications:
- Rejection
- Infections (due to immunosuppressants)
- Post-transplant lymphoproliferative disorder
- Electrolyte disturbances → Bone density loss
- Drug side effects
- Signs of Rejection:
- Biopsy: Inflammatory cell infiltrate
- Functional: Anaemia, hypertension, uraemia
Bone Marrow Transplant (BMT)
- Indications: Leukaemia, lymphoma, immunodeficiency, aplastic anaemia
- Procedure:
- High-dose chemotherapy/radiation to eliminate host marrow
- Donor marrow infused (from relative or umbilical cord)
- Key Requirements:
- HLA match
- Crossmatch
- Mixed lymphocyte culture
- Complications:
- Graft failure
- Infections
- Graft-versus-host disease (GVHD)
- Graft attacks host (even with full HLA match due to minor antigens)
- Symptoms: Fever, rash, hepatosplenomegaly, diarrhoea
- High mortality (~70%)
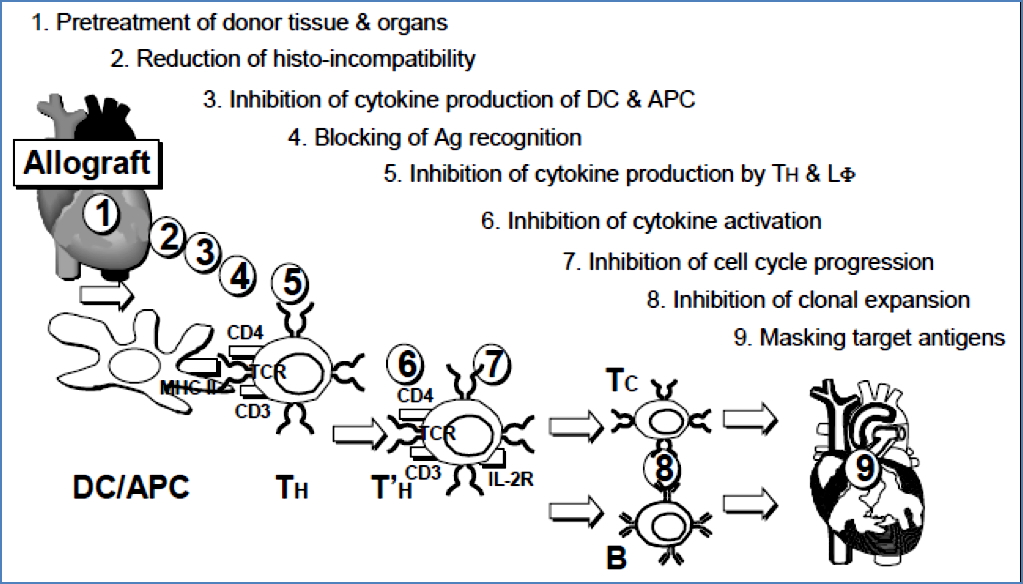
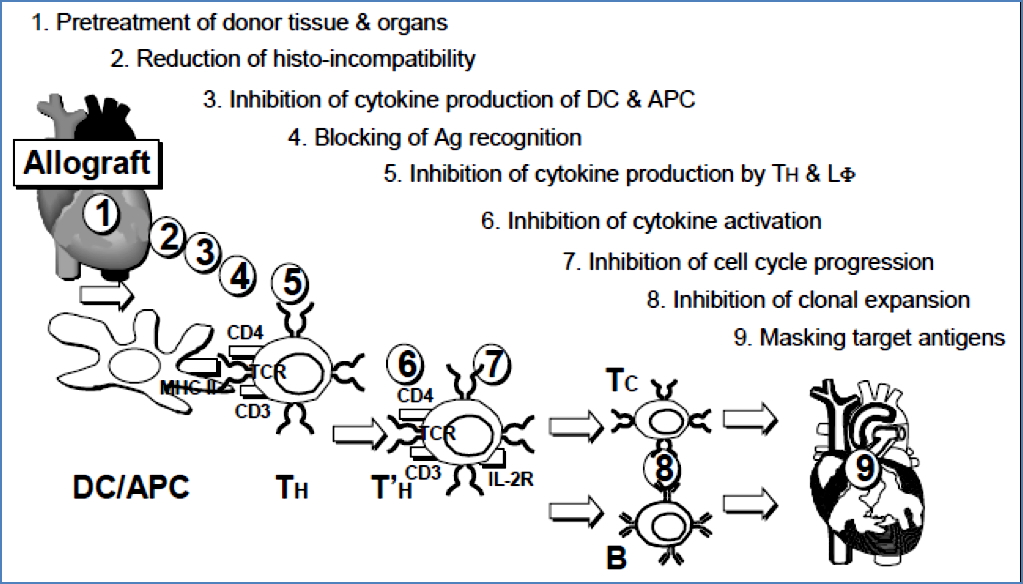
Immune Intervention in Transplantation
Types of Immune Intervention
- Immunosuppression (most common)
- Induction of tolerance (experimental)
- Pre-treatment of graft (removal of donor APCs)
Immunomodulation Targets
- Any point in antigen presentation, T-cell activation, or effector response
Immunosuppressive Therapy
Requirements
- Induction: At or before transplant
- Maintenance: Prevent long-term rejection
- Rescue: Manage acute rejection episodes
Agents
Corticosteroids (e.g. Prednisone)
- ↓ IL-1, IL-2 → ↓ T/B cell activation
- ↓ Phagocyte function, cytokines
- Side Effects: Infections, growth delay, diabetes, ulcers, Cushing’s
Cytotoxic Agents (Cytostatics)
- Block DNA synthesis in rapidly dividing cells → BM suppression
- Used in cancer and transplants
Cyclosporin & Tacrolimus
- Fungal metabolites → Block IL-2 receptor activation
- ↓ T-cell proliferation
- Side Effect: Nephrotoxicity
Monoclonal Antibodies
- Anti-IL2R antibodies inhibit lymphocyte activation
- Challenges: Antigen specificity and avoiding cross-reactivity
Summary – Transplant Immunology
Transplant immunology is essential in understanding how the immune system recognises and reacts to transplanted tissues. MHC matching, minor antigens, and T-cell mediated rejection underpin graft survival. Immunosuppressive therapy, while necessary, must balance efficacy and safety. For a broader context, see our Immune & Rheumatology Overview page.