Table of Contents
Overview – Immunity to Bacteria
Immunity to bacteria refers to the coordinated response of innate and adaptive immune systems to detect, neutralise, and eliminate bacterial pathogens. Because bacteria can exist extracellularly or intracellularly, and may secrete toxins, the immune system must engage a diverse set of mechanisms to prevent infection and tissue damage.
Definition
- Normal flora: Bacteria consistently present without causing disease
- Opportunistic infections: Occur when normal flora or environmental bacteria exploit a weakened host
- Tissue invasion mechanisms:
- Enzymatic breakdown of host tissues:
- Hyaluronidase, collagenase, elastase
- Coagulase secretion: promotes clotting for microbial protection
- Intracellular growth: Some bacteria can enter host cells and replicate in cytoplasm/nucleus
- Enzymatic breakdown of host tissues:
Bacterial Antigens (Virulence Factors)
Endotoxins
- Located in Gram-negative bacterial walls
- Example: Lipopolysaccharide (LPS)
- Recognised by Toll-like receptors on macrophages
- → Triggers cytokine release → May lead to septic shock
Other Surface Antigens
- Surface enzymes
- Flagella (H antigens)
- Adhesion pili (F antigens)
- Capsule (K antigens)
- Cell wall (O antigens)
- Cell membrane proteins
Exotoxins
- Secreted toxic proteins
- Example:
- Tetanus toxin
- Staphylococcal superantigens → Toxic shock


Innate Immunity
Phagocytosis
- By macrophages, dendritic cells, neutrophils
- Can be independent or mediated by antibodies/complement


Lysozyme
- Found in secretions (tears, saliva, mucus)
- Splits bacterial cell wall peptidoglycans → Bacterial lysis
Complement Activation (Alternative Pathway)
- C3b opsonisation → Enhances phagocytosis
- Membrane attack complex → Direct lysis
Neutrophils
- Phagocytosis of opsonised bacteria
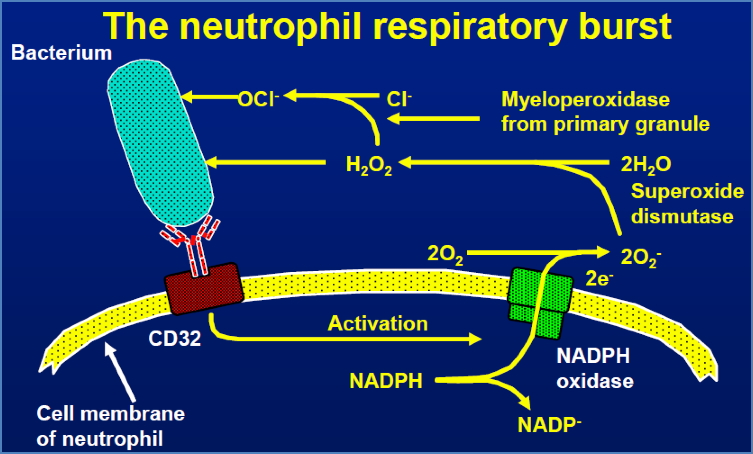
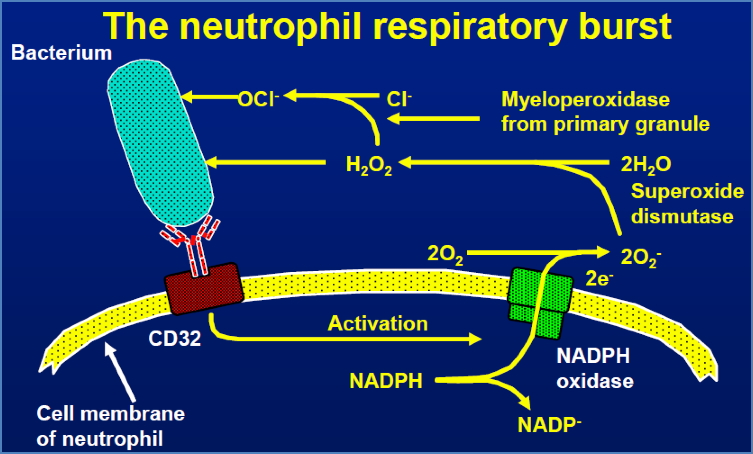
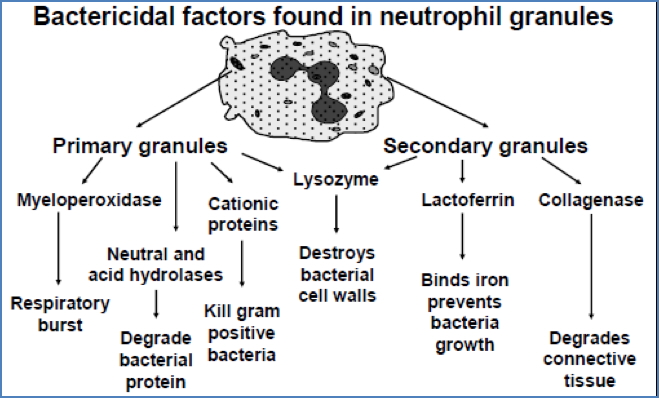
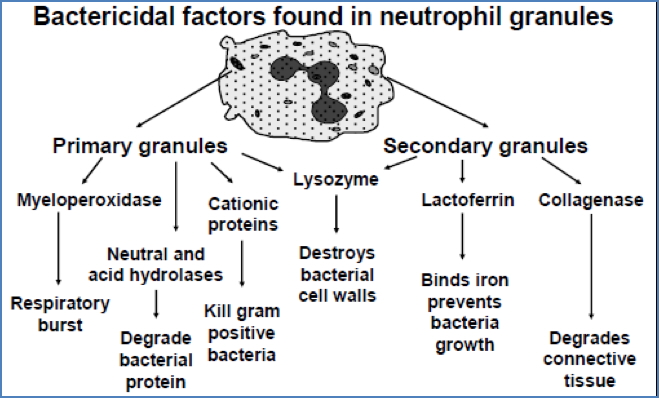
- Respiratory burst → Generates oxidative molecules that kill microbes
- Bactericidal granules
Cytokine-Mediated Inflammation
- Follows macrophage phagocytosis
- Leads to:
- Local inflammation
- Fever
- Acute phase proteins:
- C-reactive protein (CRP)
- Mannose-binding lectin (MBL)
- → Opsonisation and complement activation
Adaptive Immunity
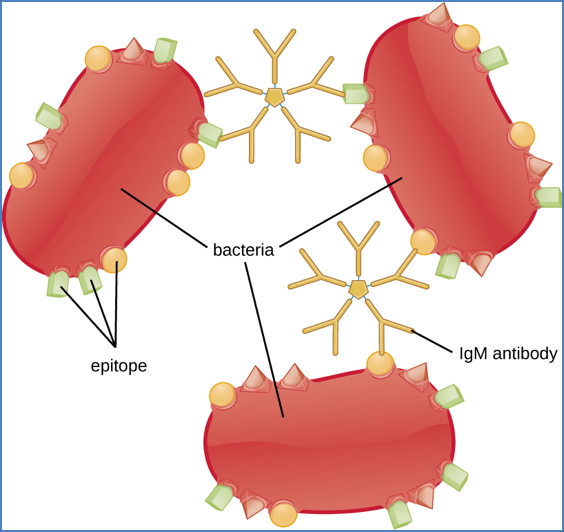
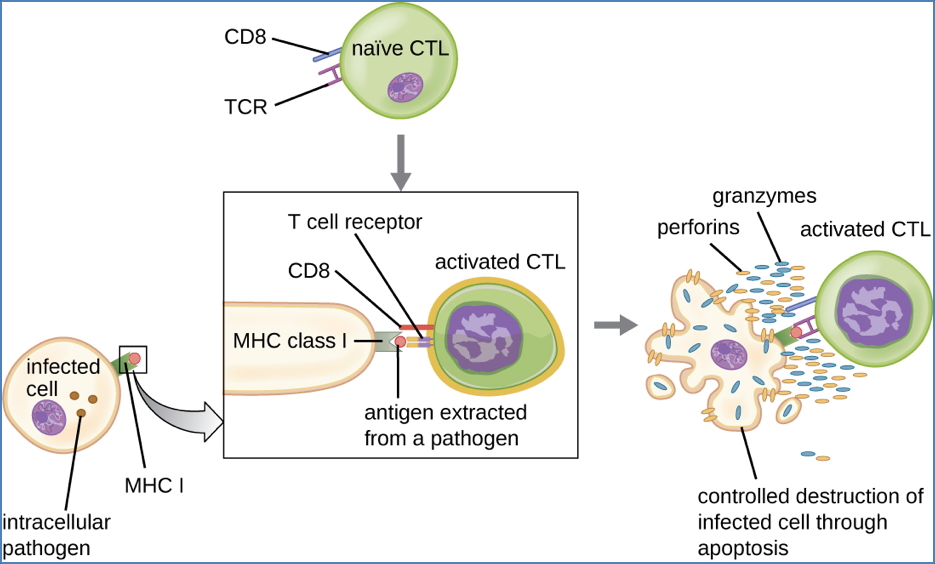
Antibodies (B-cell Mediated)
- Neutralise exotoxins (e.g. IgG binds the toxin, prevents receptor binding)
- Opsonise endotoxins and bacteria for phagocytosis
- Promote bacteriolysis
- Other antibody effects:
- Neutralisation
- Agglutination
- Antibody-dependent cell-mediated cytotoxicity (ADCC)
- Complement-mediated virolysis






CD4+ T-helper Cells
- Activate macrophages → Enhance killing of ingested bacteria
- Activate B-cells → Antibody production


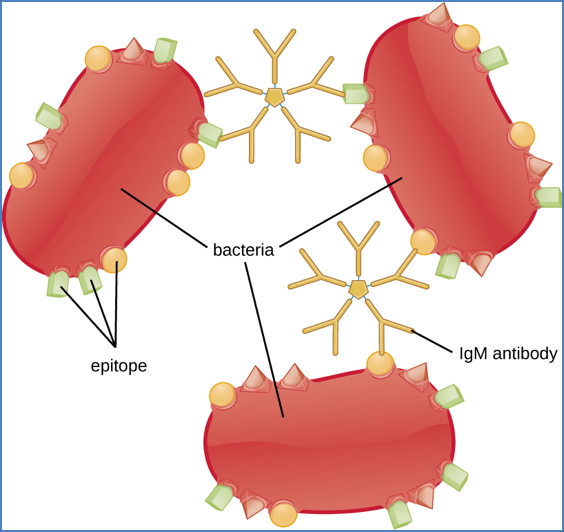
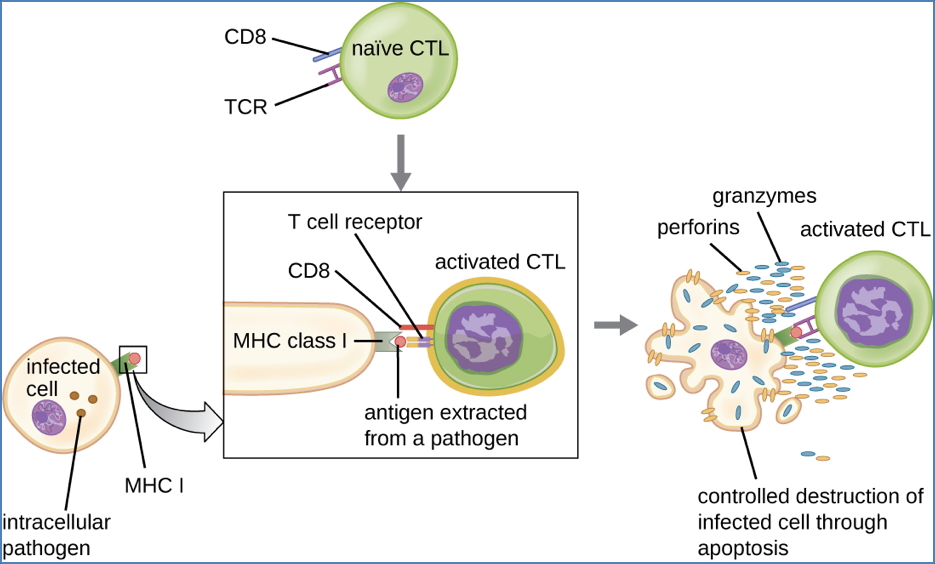
CD8+ Cytotoxic T-cells
- Recognise bacterial peptides presented on MHC-I
- Release perforins → Kill infected host cells
Mechanisms of Immune Evasion
- Antigenic variation (e.g. Neisseria gonorrhoeae, E. coli, Salmonella typhimurium)
- Complement inhibition
- Phagocytosis resistance (e.g. Streptococcus pneumoniae)
- Scavenging of reactive oxygen species (e.g. Staphylococcus aureus, Mycobacterium leprae)
- Phagolysosome inhibition (e.g. Mycobacterium tuberculosis, Legionella pneumophila)
- Phagosome escape (e.g. Listeria monocytogenes)
Summary – Immunity to Bacteria
Immunity to bacteria involves both innate and adaptive responses that together help neutralise, ingest, and destroy bacterial pathogens and their toxins. Despite these defences, many bacteria employ sophisticated strategies to evade immunity. For a broader context, see our Immune & Rheumatology Overview page.