Table of Contents
Overview – Treating Respiratory Emergencies
Treating respiratory emergencies is a critical component of acute care, often requiring rapid, structured decision-making to secure the airway, support ventilation, and address underlying pathology. Early intervention with definitive and supportive therapies can be life-saving, particularly in conditions like anaphylaxis, pneumonia, and trauma-related chest injuries.
Definition
Treating respiratory emergencies involves stabilising airway, breathing, and circulation (ABC), while also initiating targeted therapy to resolve the underlying respiratory pathology.
Definitive Treatments
These treatments directly address the underlying cause:
- Anaphylaxis → Adrenaline
- Asthma → Bronchodilators
- Pneumonia → Antibiotics
- Tension Pneumothorax → Intercostal Catheter (ICC)
Supportive Treatments
Securing the Airway
Positioning
- Jaw thrust
- Chin lift
- Head tilt
- Lateral positioning (lying on side)
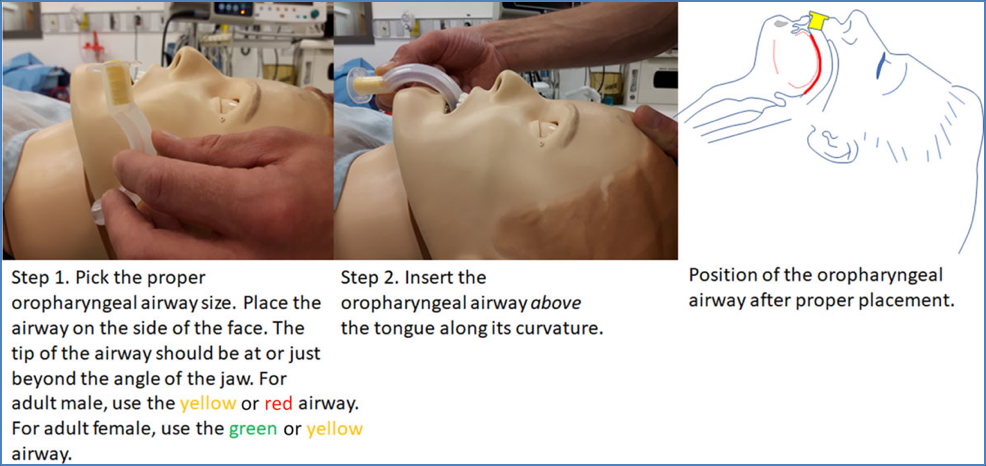
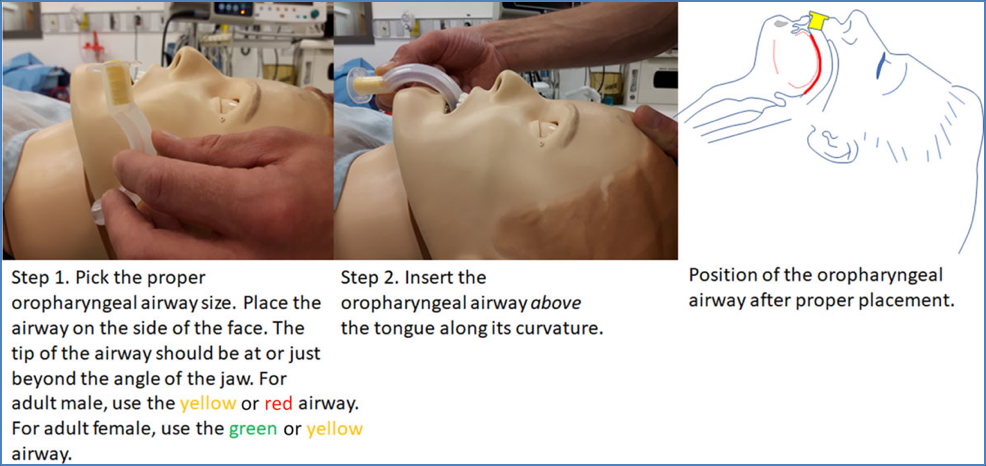
Basic Airway Adjuncts
- Oropharyngeal Airway (OPA) – Guedel airway
- Insert above the tongue using curvature
- Size selected by aligning tip to angle of jaw
- Nasopharyngeal Airway (NPA)
- Used when OPA not tolerated
- Inserted into nostril; avoids triggering gag reflex


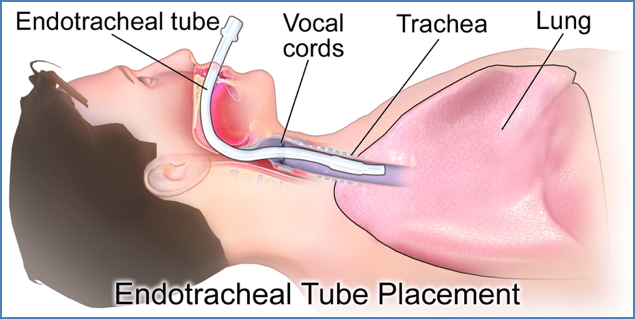
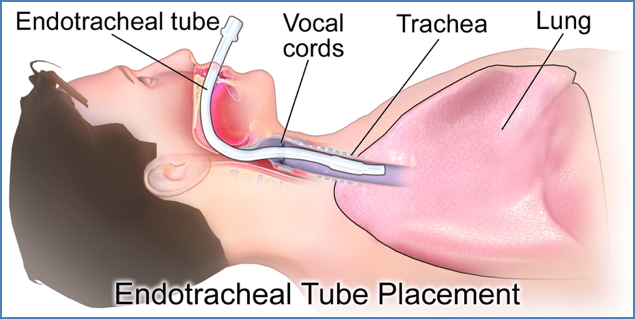
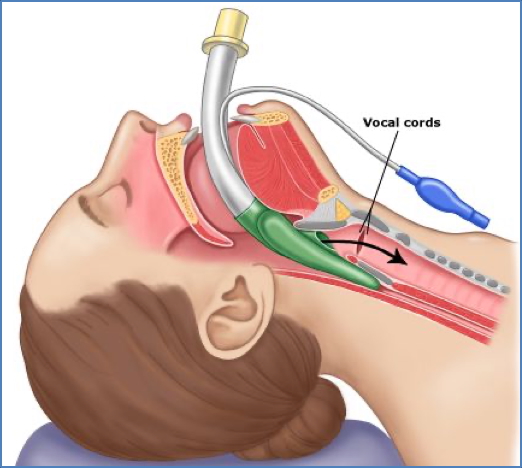
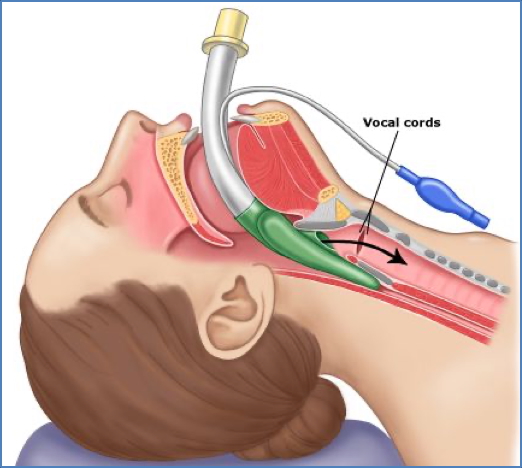
Advanced Airway Adjuncts
- Endotracheal Tube (ETT) – definitive airway
- Laryngeal Mask Airway (LMA) – used in difficult airways or during anaesthesia
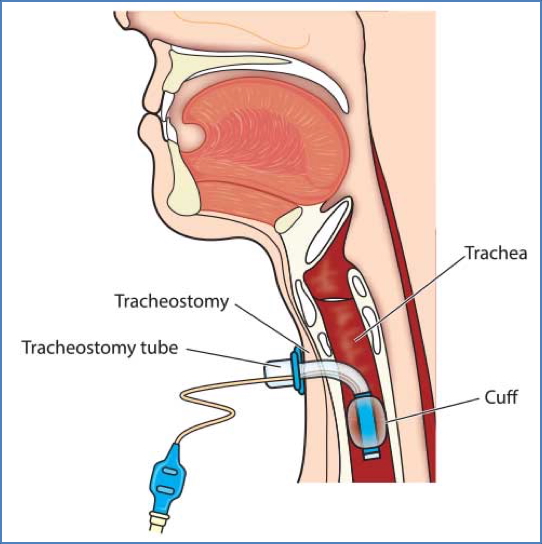
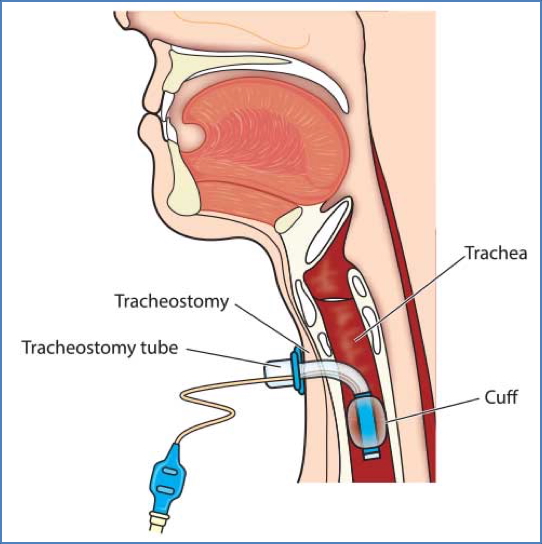
- Surgical Airway – e.g. tracheostomy, cricothyrotomy (last resort)
2. https://somepomed.org/articulos/contents/mobipreview.htm?4/1/4114
3. https://www.ausmed.com.au/cpd/articles/tracheostomy-management
Breathing Support
Increasing FiO₂
- Fraction of inspired oxygen (FiO₂) is expressed as a percentage
- Target <60% for <24 hours to avoid oxygen toxicity
Assisted Ventilation
- Indicated when respiratory drive is lost
- Requires patent airway and tight-fitting mask
Oxygen Delivery Systems
Nasal Cannulae
- Flow: 2–6 L/min → FiO₂: 0.25–0.40
- Pros: Comfortable, allows oral intake, low cost
- Cons: Variable FiO₂, drying at high flows


Hudson Mask
- Flow: 4–15 L/min → FiO₂: 0.35–0.70
- Pros: Comfortable, adaptable FiO₂
- Cons: Variable FiO₂, rebreathing risk at low flow


Venturi Mask
- Flow: 3–12 L/min → FiO₂: 0.24–0.60
- Uses Venturi principle to mix room air and oxygen
- Pros: Predictable FiO₂, no rebreathing
- Cons: Max FiO₂ 60%, performance drops with high inspiratory flow


Non-Rebreather Mask (Reservoir Mask)
- Max flow: 15 L/min → FiO₂: up to 0.85
- Pros: High FiO₂ without intubation
- Cons: Risk of rebreathing if valves fail


Bag-Valve Mask (BVM)
- Flow: 15 L/min → FiO₂ near 100%
- Indications: Apnoea or very low respiratory effort


Oxygen Use Precautions
- Oxygen Toxicity:
- FiO₂ > 0.6 for >24 hours
- Chronic Airway Limitation (CAL):
- Patients with chronic CO₂ retention may rely on hypoxic drive
- Excess oxygen can suppress respiration


Example Emergency Cases
Case 1 – Viral Infection
- 100% O₂ sats, afebrile, cough
- → Reassurance, fluids
Case 2 – Severe Pneumonia
- Febrile, crepitations, hypoxic
- → IV antibiotics, IV fluids, oxygen
Case 3 – Chest Trauma
- Knife wound, hypotensive, JVP flat
- → Suspected haemothorax
- → Chest drain with ICC
Case 4 – Hanging
- Unconscious, stridor
- → Airway priority
- → Intubation or emergency tracheostomy if failed
Case 5 – High-speed MVA
- Pale, hypotensive, L lung whited out
- → Haemothorax ± pneumothorax
- → Emergency ICC
Case 6 – Croup
- Barking cough, stridor, dyspnoea
- → Nebulised adrenaline and steroids
Arterial Blood Gas (ABG) Interpretation – Case Examples
Case 1 – Normal Student Sample
- pH 7.40, pCO₂ 40, HCO₃ 27 → Normal
Case 2 – Drug Overdose
- pH 6.95, pCO₂ 85 → Respiratory acidosis
Case 3 – Hyperventilation
- pH 7.7, pCO₂ 10 → Respiratory alkalosis
Case 4 – Diabetic Ketoacidosis
- pH 7.2, HCO₃ 14, Base Excess -12 → Metabolic acidosis
Case 5 – Diarrhoea
- pH 7.6, HCO₃ 39, Base Excess +10 → Metabolic alkalosis
Case 6 – Respiratory Failure with Compensation
- pH 7.25, pCO₂ 90, HCO₃ 38, BE +10
- → Respiratory acidosis with metabolic compensation
Summary – Treating Respiratory Emergencies
Treating respiratory emergencies requires rapid identification of the underlying cause, followed by airway management, appropriate oxygen supplementation, and targeted therapy. Mastery of airway adjuncts, oxygen delivery systems, and blood gas interpretation is essential for safe and effective care. For a broader context, see our Emergency Medicine Overview page.