Table of Contents
Overview – Assessing Respiratory Emergencies
Assessing respiratory emergencies involves rapid clinical evaluation, supported by targeted investigations to identify airway compromise, impaired ventilation, or gas exchange failure. This article provides a structured approach combining primary survey (ABC), examination, and interpretation of key diagnostic tools like pulse oximetry and arterial blood gases (ABGs). Early intervention can be life-saving in respiratory failure.
Initial Assessment – ABC
- A: Airway: Check patency, obstruction, trauma, or swelling
- B: Breathing: Rate, depth, effort, oxygen saturation
- C: Circulation: BP, pulse, signs of perfusion
In-Depth Assessment
Appearance – “End-of-the-bed” Observations
- Level of consciousness
- Sweating
- Agitation
- Cyanosis or pallor
- Urticaria or angioedema
History
- Onset and progression of symptoms
- Nature of symptoms (e.g. dyspnoea, cough, wheeze)
- Associated features (e.g. fever, chest pain)
- Past episodes and treatment so far
- Relevant past medical history
Examination
- Respiratory rate (most sensitive vital sign in deterioration)
- Airway patency: Look for obstruction, stridor, swelling
- Work of breathing: Use of accessory muscles, nasal flaring
- Auscultation: Air entry, wheezes, crackles
- Percussion: Hyperresonance or dullness
- Tracheal deviation
- Jugular venous pressure (JVP)
- Pulse and blood pressure
Monitoring
- Oxygen saturation (SpO₂)
- Full set of vital signs
Investigations
- Arterial blood gas (ABG)
- Chest X-ray
- ECG
- Spirometry (when stable)
- Sputum culture
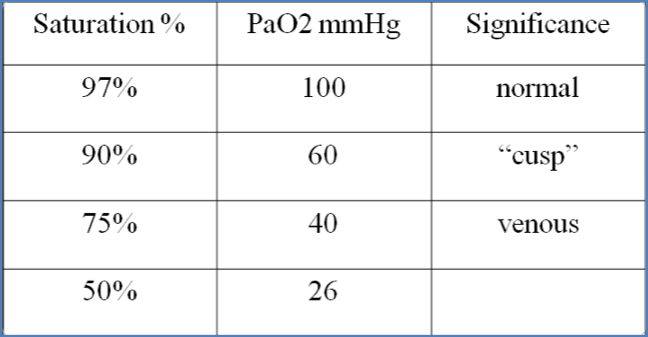
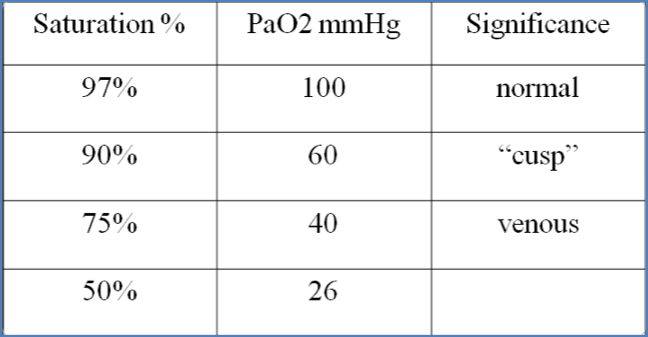
Pulse Oximetry – Key Concepts
- Higher O₂ saturation = higher arterial pO₂
- Based on the oxygen-haemoglobin dissociation curve:
- Plateau phase favours O₂ loading
- Steep phase favours O₂ unloading in tissues
Factors That Shift the Curve
- Right shift (favouring O₂ unloading):
- Acidosis (↓pH)
- Hypercapnia (↑pCO₂) – Bohr effect
- Raised 2,3-BPG (seen in hypoxia)
- Hyperthermia (e.g. exercise)
Clinical Implications of Arterial pO₂
- 90 mmHg: Normal
- ~55 mmHg: Euphoria, memory loss
- 30–55 mmHg: Loss of cognitive/motor function
- <30 mmHg: Unconsciousness
Arterial Blood Gas (ABG) Analysis
What ABGs Tell Us
- Oxygenation: PaO₂
- Ventilation: PaCO₂
- Acid–base status: pH, HCO₃⁻, base excess
- A-a gradient: Identifies gas exchange abnormalities
Normal Values
| Parameter | Normal Range |
|---|---|
| pH | 7.35–7.45 |
| pO₂ | 70–100 mmHg |
| pCO₂ | 35–45 mmHg |
| HCO₃⁻ | 22–26 mmol/L (arterial) |
| Base Excess | -3 to +3 |
Interpreting Acid-Base Disturbance
Acidosis
- pH < 7.35
- Respiratory acidosis: Hypoventilation → ↑pCO₂
- Compensation: Renal HCO₃⁻ retention
- Metabolic acidosis: Loss of HCO₃⁻ or gain of acid
- Compensation: Hyperventilation (↓pCO₂)
Alkalosis
- pH > 7.45
- Respiratory alkalosis: Hyperventilation → ↓pCO₂
- Compensation: Renal HCO₃⁻ excretion
- Metabolic alkalosis: H⁺ loss or excess base
- Compensation: Hypoventilation (↑pCO₂)
Buffer System Recap
- Bicarbonate buffer:
H⁺ + HCO₃⁻ ⇌ H₂CO₃ ⇌ CO₂ + H₂O - Acidosis: Add HCO₃⁻ or reduce CO₂
- Alkalosis: Add H⁺ or raise CO₂
Anion Gap
- AG = [Na⁺] – ([Cl⁻] + [HCO₃⁻])
- High AG Metabolic Acidosis:
- Lactic acidosis
- Ketoacidosis
- Renal failure
- Normal AG Metabolic Acidosis:
- GI loss (diarrhoea)
- Renal loss (renal tubular acidosis)
A-a Gradient
- A-a Gradient = Alveolar pO₂ – Arterial pO₂
- Normal value: <12 mmHg
- Elevated gradient → V/Q mismatch (e.g. PE, pneumonia, fibrosis)
6-Step ABG Interpretation Strategy
- Assess pH: Acidosis or alkalosis?
- Check pCO₂: Is it consistent with the pH?
- Check HCO₃⁻: Metabolic contribution?
- Identify primary disturbance
- Evaluate compensation:
- Base excess
- Respiratory/metabolic signs of adjustment
- Summarise your findings
Summary – Assessing Respiratory Emergencies
Assessing respiratory emergencies involves a structured approach to appearance, examination, and investigation. Tools like ABG analysis and pulse oximetry help differentiate between ventilation and oxygenation problems, enabling rapid, targeted management. For a broader context, see our Emergency Medicine Overview page.