Table of Contents
Overview – Assessing Cardiovascular Emergencies
Assessing cardiovascular emergencies is a critical skill that involves rapid identification of life-threatening conditions, stabilisation, and targeted investigation. From shock to acute myocardial infarction (AMI), a structured approach ensures appropriate diagnosis, triage, and timely intervention. This article outlines a high-yield framework for recognising severity and cause, guiding management in emergency settings.
Aims of Assessment
- Determine the cause of cardiovascular instability
- Determine the severity and urgency of the condition
Approach to Assessment
1. Immediate ABC Survey – 30-Second Exam
- Airway
- Breathing
- Circulation
- Immediate stabilisation of life-threatening abnormalities
2. Stabilisation
- Control haemorrhage
- Support oxygenation and perfusion
- Initiate cardiac monitoring
3. Detailed Assessment
Appearance
- Level of consciousness
- Sweating, agitation
- Cyanosis or pallor
- Visible external bleeding
- Chest-clutching or other clues to underlying pathology
History
- Nature, onset, and progression of symptoms
- Associated symptoms
- Any treatment already given
- Previous episodes or known cardiac history
Cardiovascular Examination
Pulse
- Rate
- Rhythm
- Volume
- Peripheral vs central location
Blood Pressure
- Know the patient’s baseline
- Define what’s low or elevated for them
- Measure accurately (e.g. manual cuff, both arms if shock suspected)
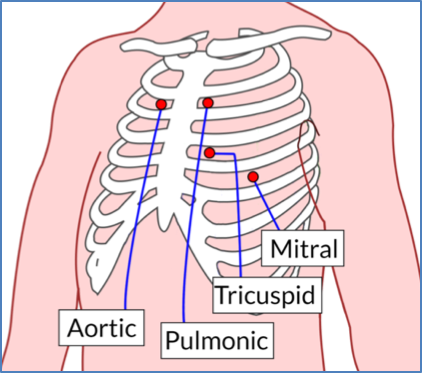
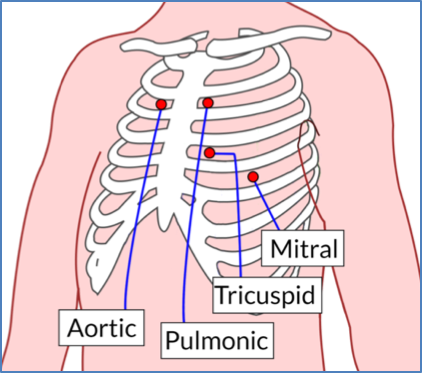
Heart Examination
- Heart sounds (e.g. murmurs, gallops)
- Capillary refill time:
- Peripheral: Nail bed blanching <2 seconds = normal
- Central: Assess over sternum
- Signs of heart failure:
- Raised jugular venous pressure (JVP)
- Peripheral oedema
- Pulmonary crepitations
- Signs of chronic cardiovascular disease
Monitoring and Investigation
Monitoring
- Direct indicators:
- ECG
- Continuous blood pressure and pulse
- Indirect indicators:
- Oxygen saturation
- Urine output (renal perfusion)
- Glasgow Coma Scale (GCS) for cerebral perfusion
Investigations
- ECG: Rhythm abnormalities, ST changes, evidence of ischaemia
- Chest X-ray: Pulmonary oedema, cardiomegaly
- Echocardiography: Structural/functional assessment
- Blood tests:
- Troponins
- Electrolytes
- Full blood count
- Coagulation profile
Interpreting Your Assessment
By the end of assessment, you should have:
- An idea of the likely cause (e.g. shock, hypertensive crisis, arrhythmia)
- A sense of severity to guide urgency of intervention
Important: Address any problems as they are identified during the primary survey.
Management of Cardiovascular Emergencies
Supportive Treatment
Goal: Maintain adequate tissue perfusion
- Control external bleeding
- Restore circulating volume (e.g. IV fluids)
- Improve oxygen delivery (e.g. supplemental O₂)
- Symptom relief (e.g. GTN spray for angina)
Definitive Treatment
Goal: Address the underlying pathology
- Surgery (e.g. splenectomy in trauma)
- Pacemaker insertion (e.g. for complete heart block)
- Coronary reperfusion (e.g. thrombolysis or PCI in AMI)
- Long-term pharmacological control (e.g. antihypertensives)
Supportive Interventions
Intravenous Access
- Peripheral cannulation: Various sizes/sites
- Central venous access: Subclavian, internal jugular, or femoral routes
- Other access:
- Intraosseous (IO) access in emergencies
- Umbilical veins (neonatal care)
Intravenous Fluids
- Crystalloids: Electrolyte-based solutions
- Colloids: Protein-containing (less commonly used)
- Blood products: For major haemorrhage
Medications
- Inotropes/chronotropes: For contractility and heart rate
- Antiarrhythmics or pacing: In arrhythmia management
- Diuretics: In pulmonary oedema
- Oxygen therapy: To improve arterial oxygen content
Summary – Assessing Cardiovascular Emergencies
Assessing cardiovascular emergencies requires swift evaluation of symptoms, vital signs, and perfusion status, supported by targeted investigation. Stabilising the patient while identifying the underlying cause is central to management. For a broader context, see our Emergency Medicine Overview page.