Table of Contents
Overview – Lower Limb Neurological Examination
The lower limb neurological examination is an essential OSCE skill that helps identify and localise central and peripheral nervous system lesions. It assesses tone, power, reflexes, coordination, sensation, and gait, and is key to diagnosing conditions such as multiple sclerosis, sciatica, cauda equina syndrome, and peripheral neuropathy. A systematic, bilateral approach provides valuable clinical clues, especially in stroke, spinal cord lesions, and compressive neuropathies.
General Setup
- Wash hands, introduce yourself, confirm patient’s name and age.
- Explain procedure, gain consent.
- Patient in shorts, lying at 45°, both legs exposed.
- Compare both limbs throughout.
- Around bed: check for mobility aids, medications, diabetic supplies.
- Observe patient’s posture, speech, and overall alertness.
Inspection
- Muscle wasting, fasciculations
- Asymmetry, scars, deformities
- Abnormal posturing: e.g. hemiplegia (extended, plantarflexed leg)
- Involuntary movements
- Floppy limbs (hypotonia)
Tone
- Roll thighs side to side to assess tone.
- Lift the knee sharply — in hypertonia, the foot lifts off the bed.
- Check for ankle clonus (>3 beats = sustained clonus, seen in UMN lesions).
Power (MRC Grading 0–5)
Test with muscle isolation and compare sides:
- Hip:
- Flexion: Iliopsoas – Iliofemoral nerve (L1–L2)
- Extension: Gluteus maximus – Sciatic nerve (L5–S1)
- Knee:
- Flexion: Hamstrings – Sciatic nerve (L5–S1)
- Extension: Quadriceps – Femoral nerve (L3–L4)
- Ankle:
- Dorsiflexion: Tibialis anterior – Deep peroneal nerve (L4–L5)
- Plantarflexion: Gastrocnemius and soleus – Tibial nerve (S1–S2)
- Great toe:
- Dorsiflexion: Extensor hallucis longus – Deep peroneal nerve (L5)
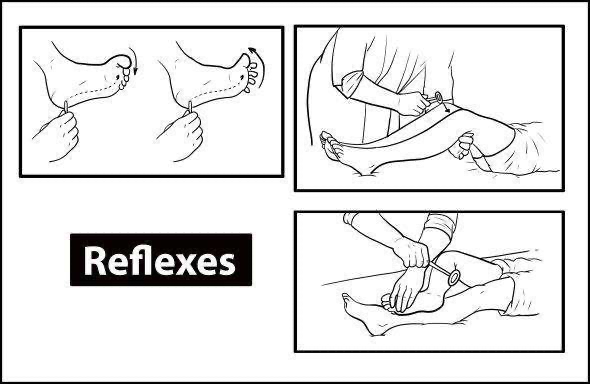
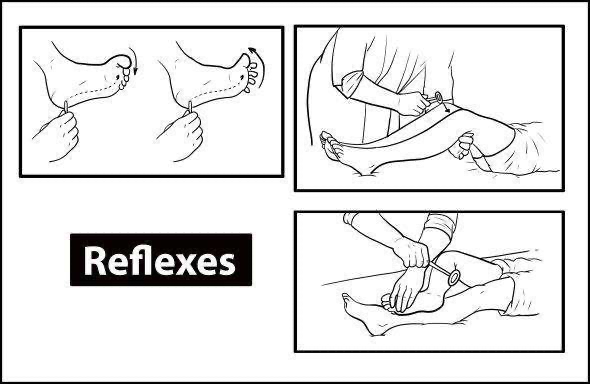
Reflexes
Use reinforcement (fingers interlocked and pulled apart) if needed:
- Knee jerk (L3–L4) – Quadriceps
- Ankle jerk (S1) – Gastrocnemius
- Plantar reflex (L5–S2) – Babinski positive = dorsiflexion of big toe (UMN sign)
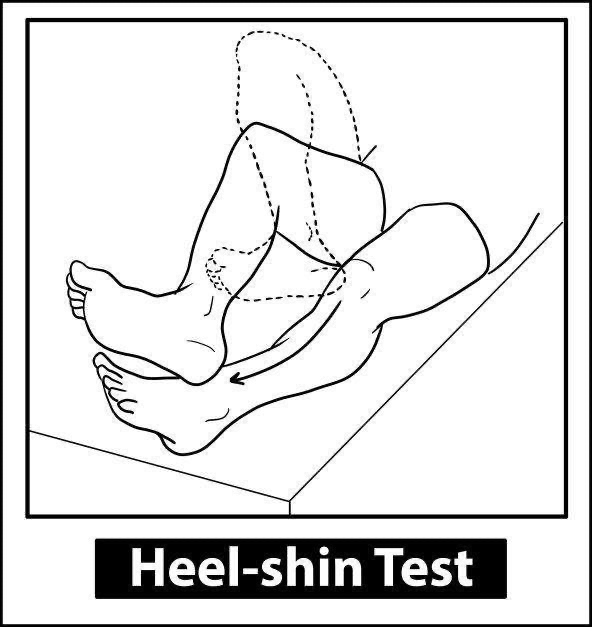
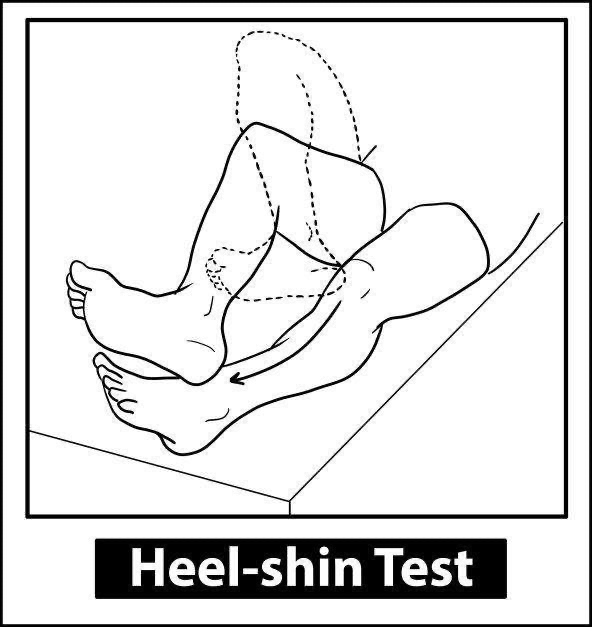
Coordination
- Heel-shin test: run heel down opposite shin
- Foot tapping: assess for cerebellar dysfunction
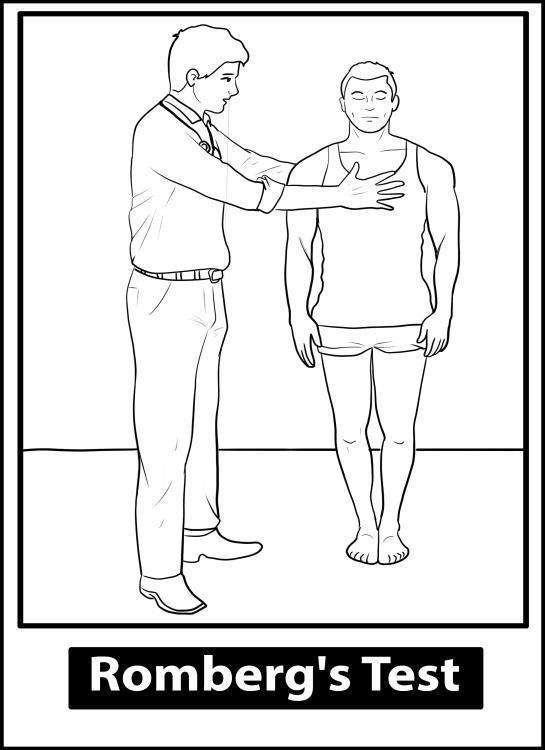
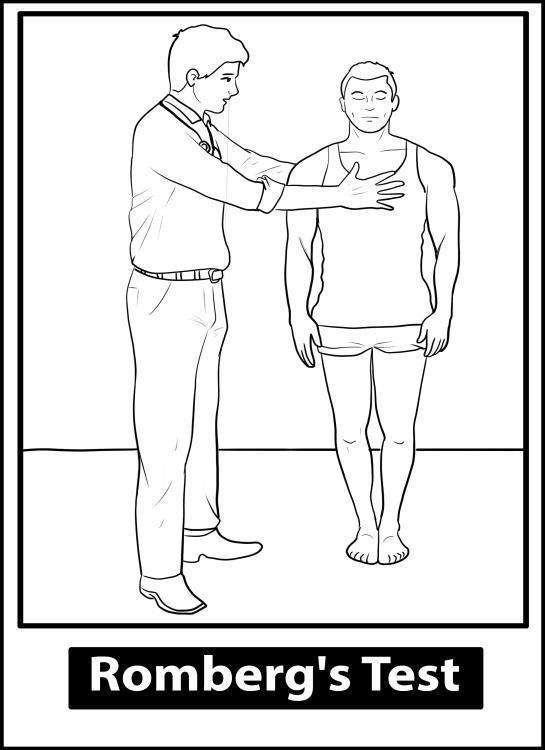
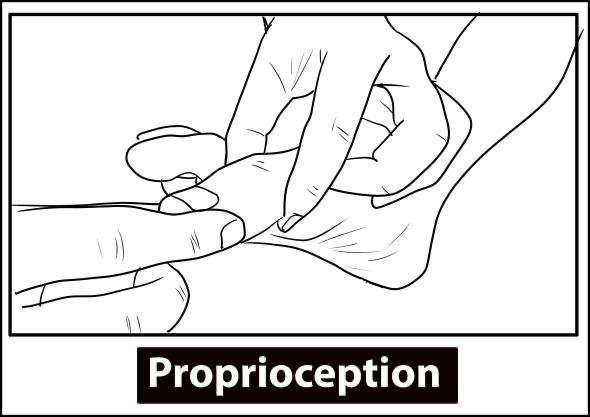
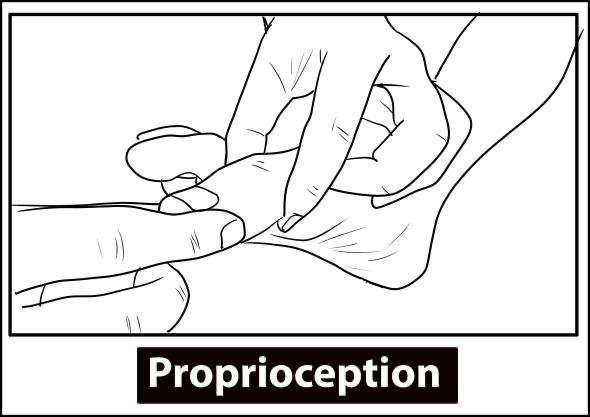
- Romberg’s test:
- Patient stands with feet together, eyes closed.
- Positive if balance is lost (indicates proprioceptive or vestibular dysfunction)
Gait Assessment
Observe while walking normally, then:
- Broad-based gait: cerebellar ataxia
- Shuffling gait: Parkinson’s disease
- Hemiplegic gait: circumduction on affected side
- High-stepping gait: foot drop
- Walk on heels: tests L4–L5
- Walk on tiptoes: tests S1–S2
- Heel-to-toe walking: cerebellar function
Special Tests
- Straight-leg raise test:
- Supine patient, leg raised with extended knee.
- Positive = sciatica-like pain → lumbar disc herniation (L5–S1)
- Anal reflex and saddle anaesthesia: for cauda equina syndrome
Associated Conditions
1. Sciatica
- Shooting radicular pain (buttock → foot), worsens with coughing/sneezing.
- LMN signs: weakness, flaccid tone, reduced reflexes.
- Causes:
- L5–S1 disc herniation
- Spinal stenosis
- Tumour, abscess
- Spondylolisthesis
- Pregnancy
2. Cauda Equina Syndrome
- Sciatica symptoms +
- Urinary/fecal incontinence or retention
- Saddle anaesthesia
- Sexual dysfunction (impotence)
- Due to:
- Massive disc herniation
- Spinal stenosis
- Tumour, abscess, haematoma
3. Subacute Combined Degeneration (SCD)
- Due to vitamin B12 deficiency (pernicious anaemia, Crohn’s disease)
- Loss of proprioception and vibration (dorsal column)
- Spasticity (corticospinal tract)
- May show cerebellar signs
4. Multiple Sclerosis (MS)
- Eye signs: optic neuritis, INO, diplopia
- Cerebellar signs, autonomic dysfunction
- Uhthoff phenomenon (worsening with heat), Lhermitte’s sign
- Investigations:
- MRI (T2 lesions)
- CSF: oligoclonal bands
- Treatment:
- Methylprednisolone (acute)
- Beta-interferon, natalizumab (long-term)
- Symptom control: baclofen (spasticity), buspirone (tremor), cholinesterase inhibitors (incontinence)
5. Diabetic Foot
| Neuropathic | Ischemic |
|---|---|
| Warm, dry, pink foot | Cold, shiny, hairless foot |
| Pulses normal | Pulses diminished |
| Reduced sensation | Painful ulcers |
| Absent Achilles reflex | Ulcer pain present |
Summary – Lower Limb Neurological Examination
The lower limb neurological examination is a vital component of OSCEs used to assess tone, power, reflexes, sensation, and gait. It helps differentiate upper versus lower motor neuron lesions and localise pathologies such as sciatica, cauda equina syndrome, multiple sclerosis, and peripheral neuropathy. For a broader context, see our Clinical Skills Overview page.