Table of Contents
Overview – Haemostasis
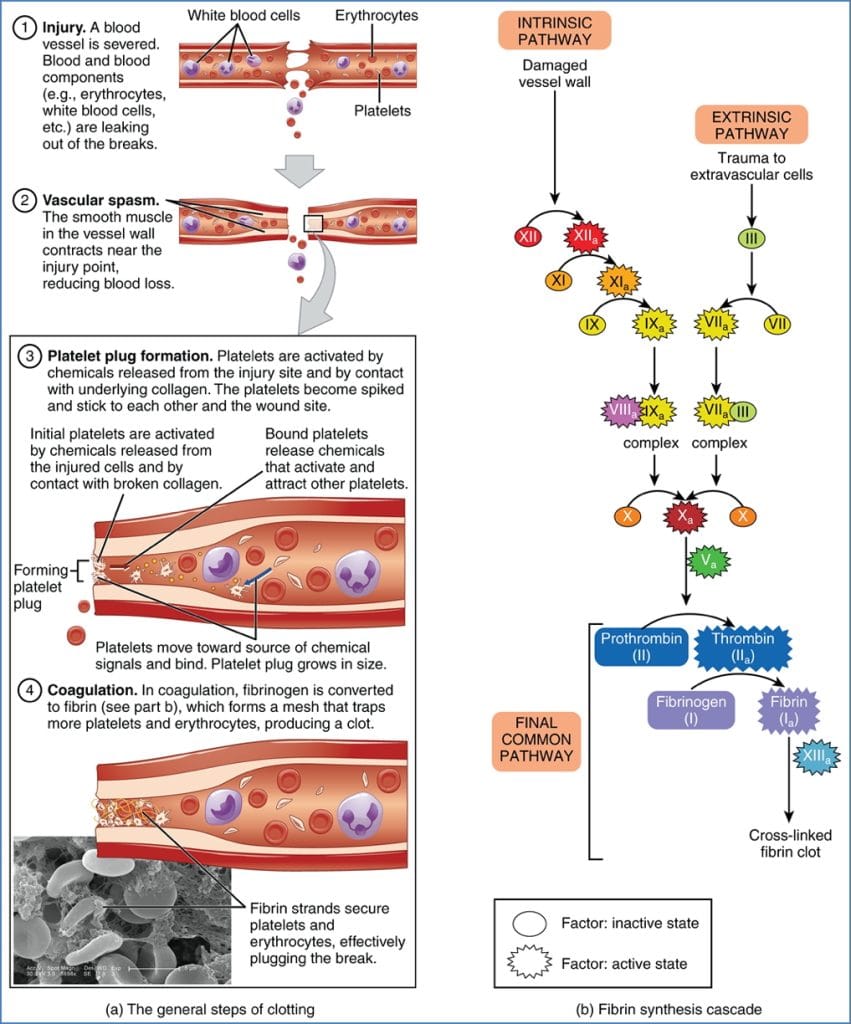
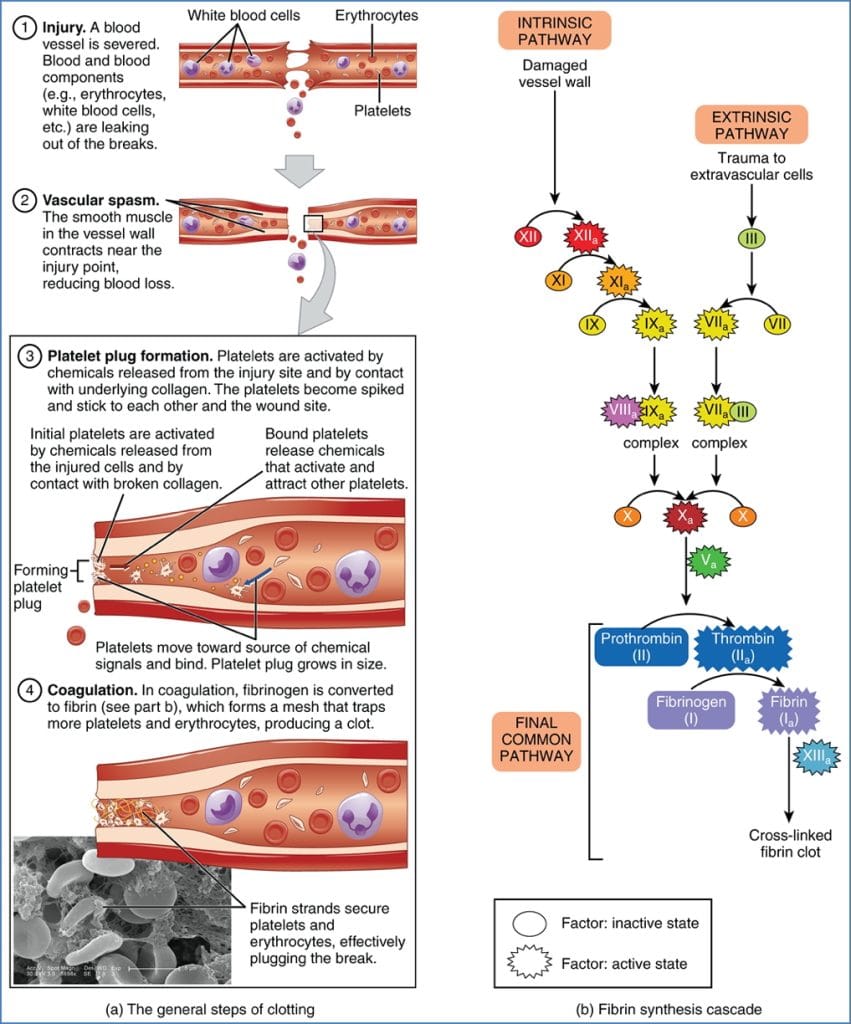
Haemostasis (or hemostasis) refers to the body’s finely tuned mechanism for halting bleeding following vascular injury. Without it, even minor cuts would lead to uncontrolled blood loss. It involves rapid, localised responses that include vascular spasm, platelet plug formation, and activation of the coagulation cascade — culminating in a stable fibrin clot. Understanding haemostasis is crucial for interpreting bleeding disorders, anticoagulant use, and clotting test results in clinical settings.
Definition
- Haemostasis = the physiological process that stops bleeding
- Involves:
- Vascular spasm
- Platelet plug formation
- Coagulation cascade
- Results in: a stable fibrin clot at the site of injury
Key Components
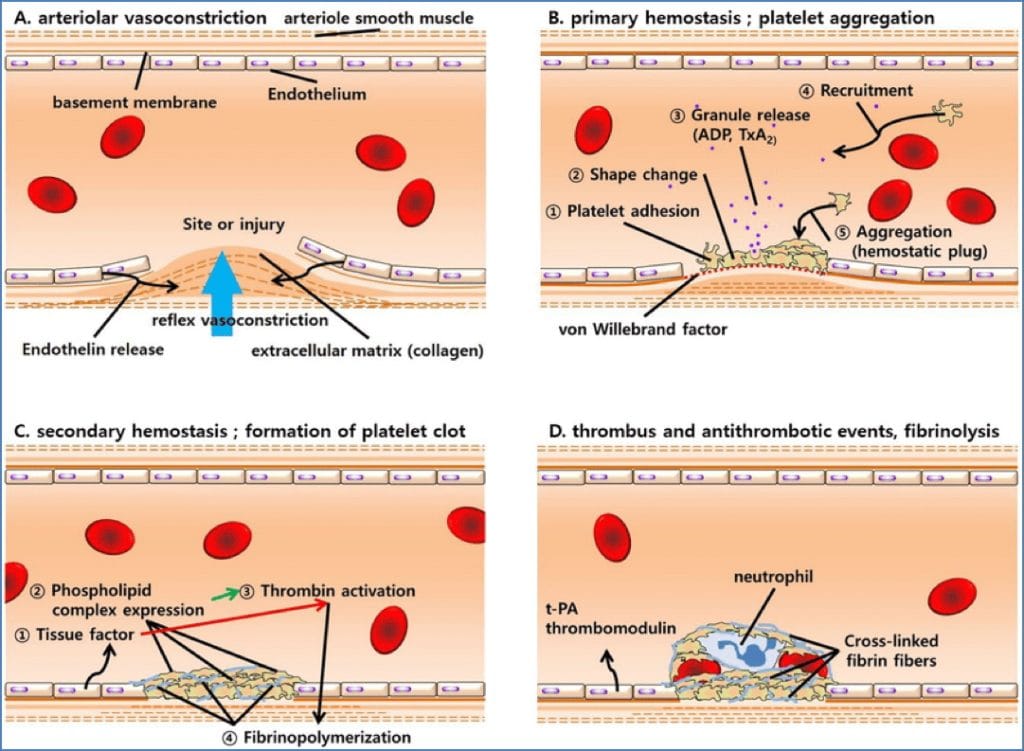
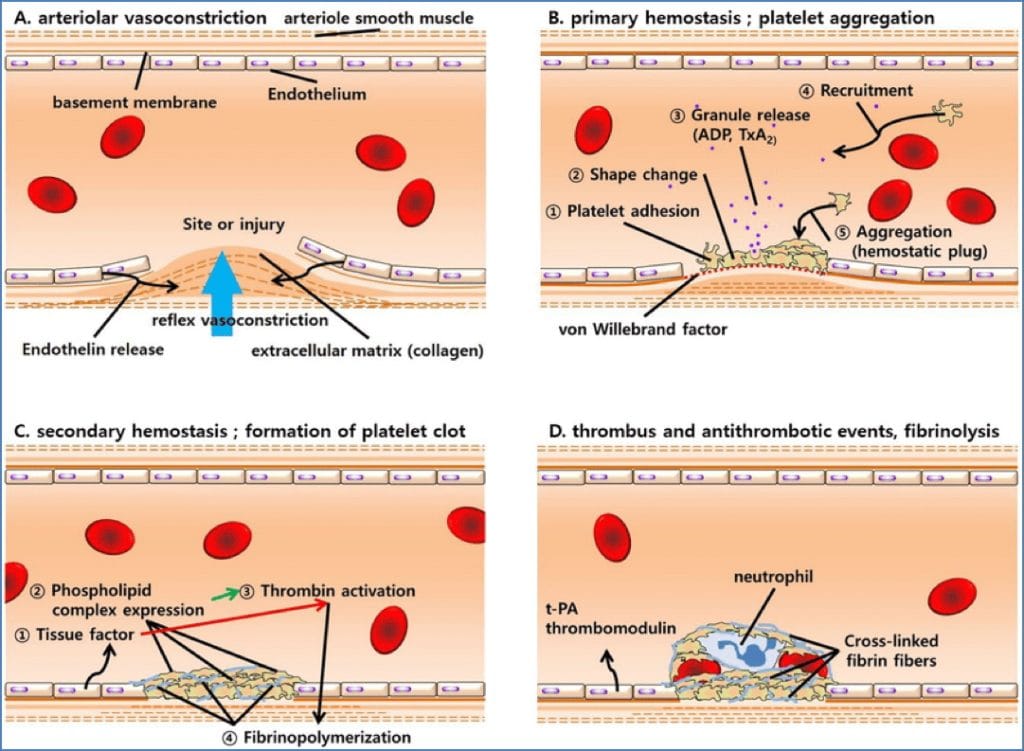
Endothelial Cells
- Line all blood vessels (simple squamous epithelium)
- Normal role:
- Barrier between blood and tissue
- Fluid regulation, immune cell migration, angiogenesis
- When injured:
- Expose subendothelial collagen → activates platelets
- Produce von Willebrand factor (vWF) – glue for platelet adhesion
- Express tissue factor (TF) – triggers extrinsic coagulation
- Block fibrinolysis (↓ tissue plasminogen activator)
- When intact:
- Release NO, heparin, thrombomodulin – inhibit clotting
- Promote fibrinolysis via tissue plasminogen activator (tPA)
Platelets
- Anuclear fragments derived from megakaryocytes
- Stimulated by thrombopoietin (from liver and kidneys)
- Central in primary haemostasis
- Aggregate and form the initial platelet plug


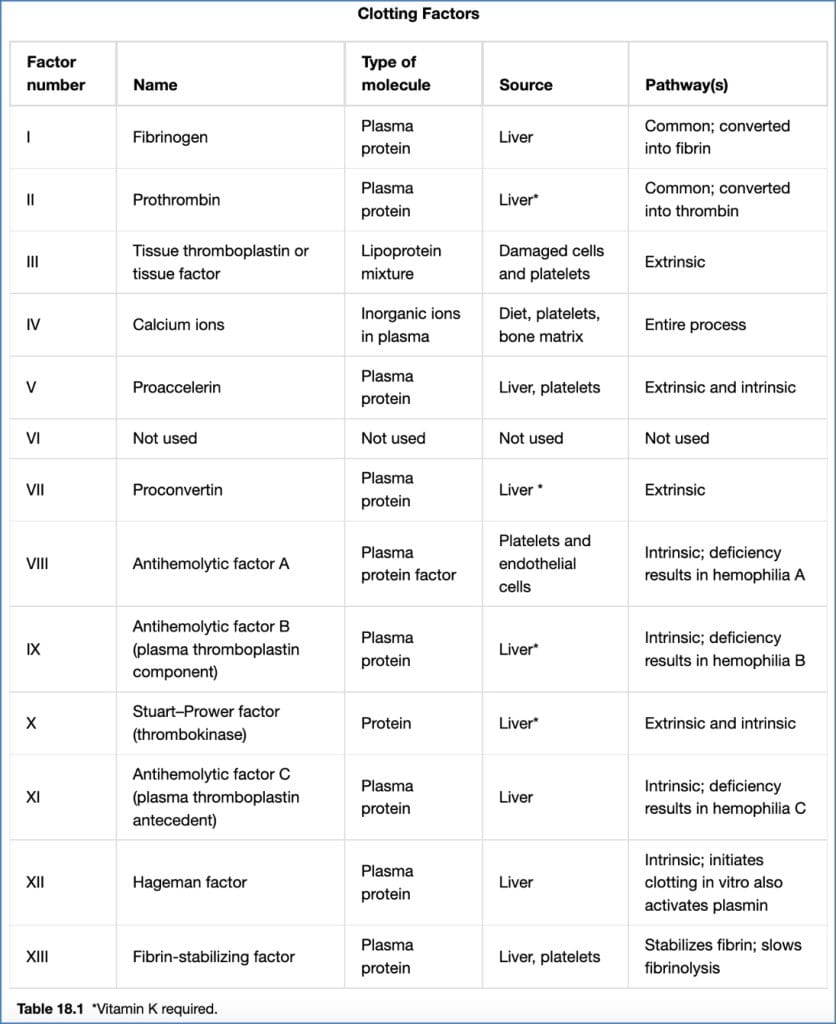
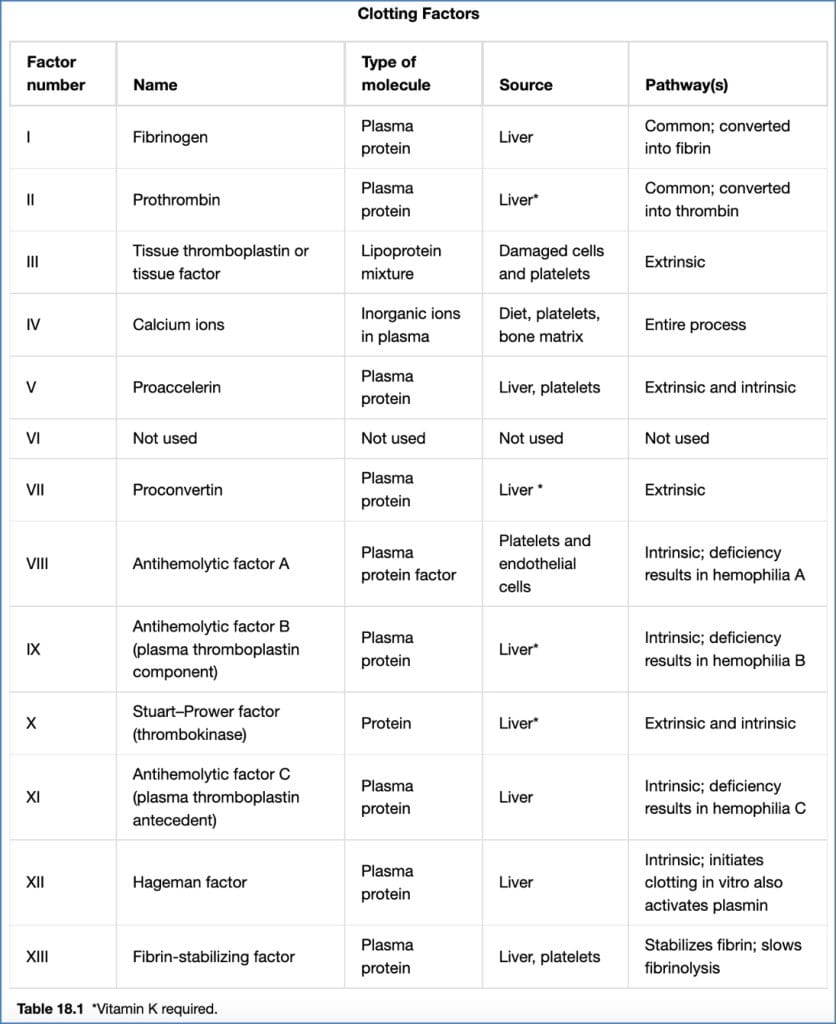
Coagulation Factors
- Mainly liver-produced, circulating in inactive form
- Convert platelet plug into a stable fibrin clot
- Pathways:
- Intrinsic: triggered by collagen exposure
- Extrinsic: triggered by tissue factor
- Common: convergence leads to fibrin formation
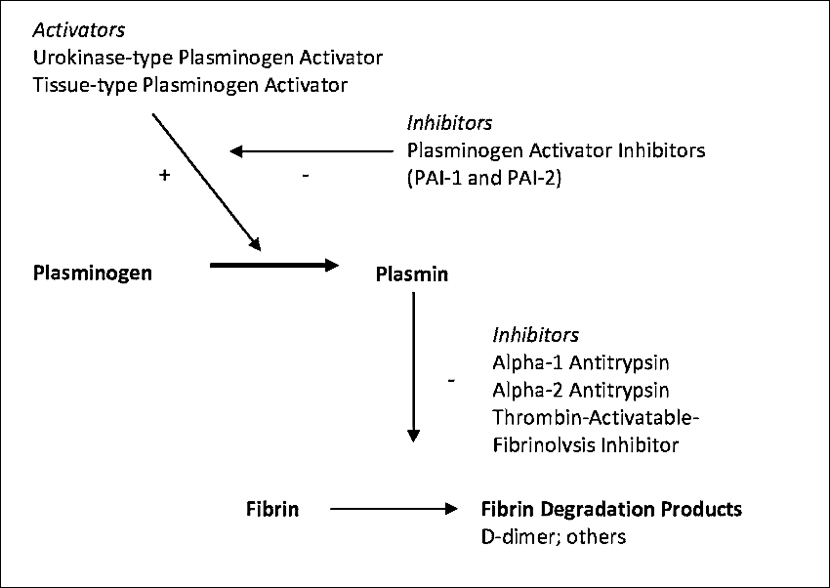
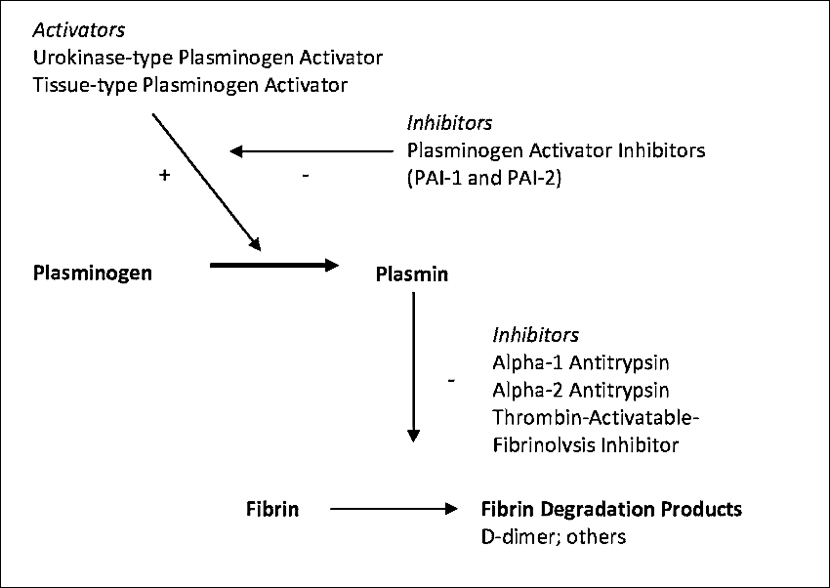
Fibrinolysis
- Removes unneeded clots after healing
- Mediated by plasmin, activated from plasminogen
- Triggered by:
- tPA (endothelial cells)
- Activated Factor XII
- Thrombin
- Results in fibrin degradation products (FDPs) — e.g., D-dimer


The 3 Phases of Haemostasis
Phase 1 – Primary Haemostasis
a) Vascular Spasm
- Immediate vasoconstriction following vessel injury
- Triggered by:
- Neural reflexes
- Endothelial signals
- Direct smooth muscle trauma
- Limits blood loss to enable clot formation
b) Platelet Plug Formation
- Platelets adhere to subendothelial collagen via vWF
- Undergo activation:
- Swell
- Form spiky projections
- Become sticky
c) Platelet Aggregation
- Activated platelets release:
- ADP – enhances aggregation
- Serotonin – vasoconstriction
- Thromboxane A2 – vasoconstrictor + aggregator
- Calcium (Factor IV) – activates other factors
- Rapid positive feedback → plug formed within 1 min
d) Localisation of Plug
- Prostacyclin (from intact endothelium) inhibits excessive aggregation


Phase 2 – Secondary Haemostasis
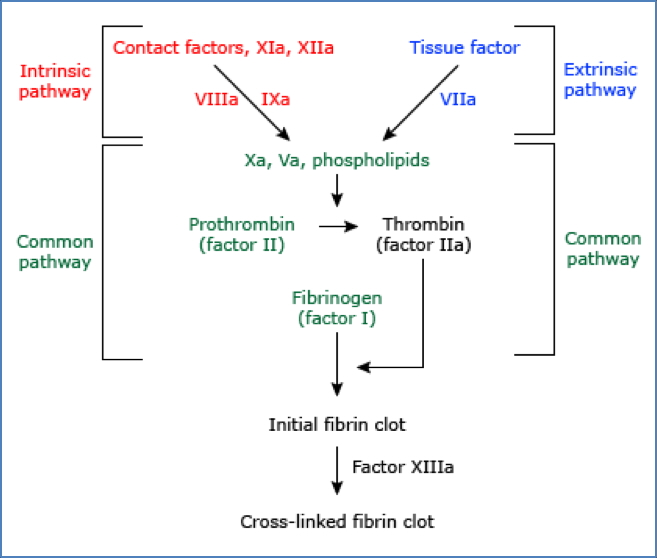
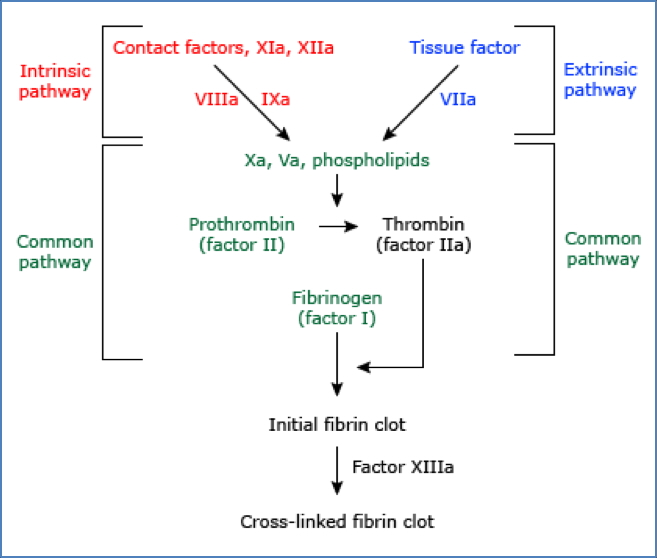
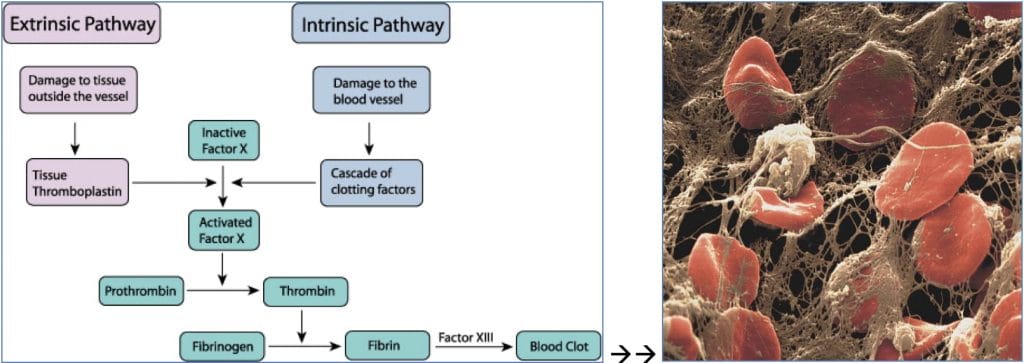
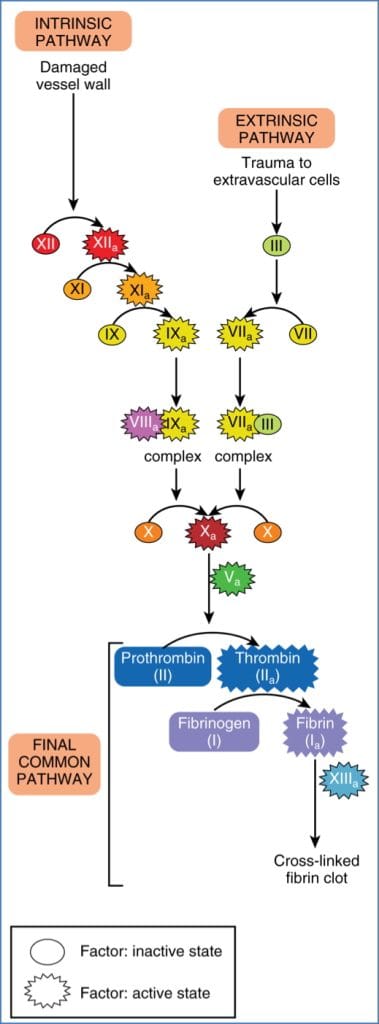
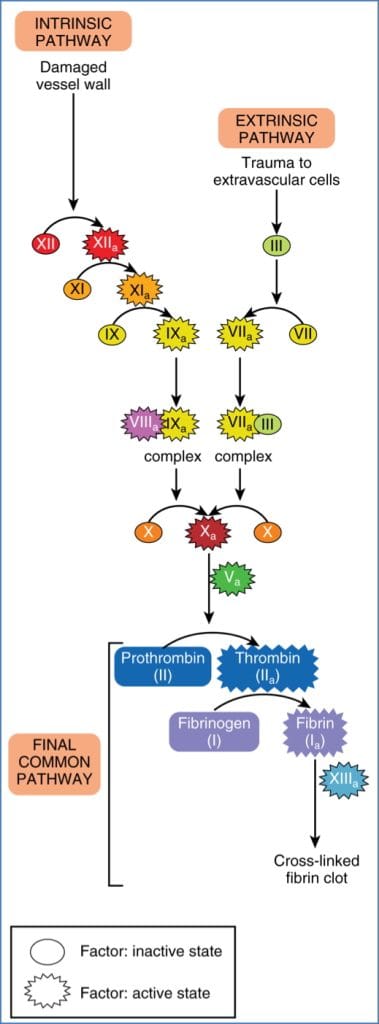
a) Coagulation Cascade
- Converts liquid blood into gel-like clot
- Enzymatic activation of clotting factors
- Intrinsic Pathway: all factors already in blood (triggered by collagen)
- Extrinsic Pathway: tissue factor exposed by injury
- Both converge to form the common pathway:
- Activation of Factor X
- Forms prothrombin activator
- Converts prothrombin (Factor II) → thrombin
- Thrombin converts fibrinogen (Factor I) → fibrin
- Factor XIII stabilises fibrin mesh → secondary platelet plug
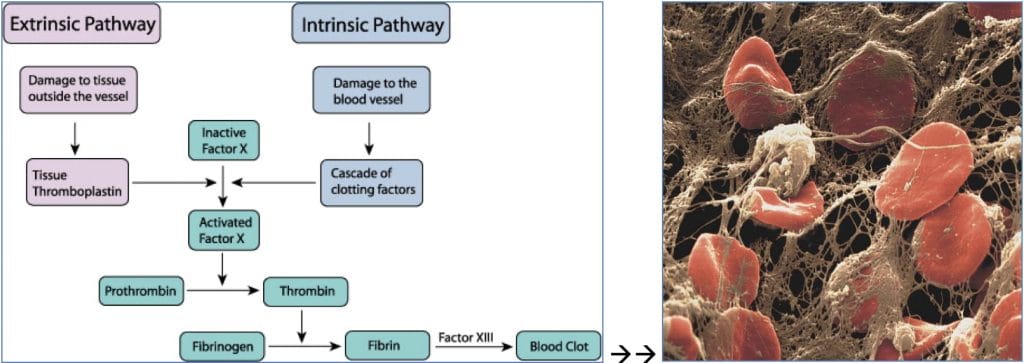
b) Regulation
- Procoagulants: Factors I–XIII (mostly inactive liver proteins)
- Anticoagulants:
- Tissue Factor Pathway Inhibitor: blocks Factor VIIa/TF complex
- Thrombomodulin: binds thrombin, activates Protein C
- Protein C & S: inactivate Factors Va & VIIIa
- Antithrombin: inhibits thrombin and Factor Xa (↑ by heparin)
c) Localisation
- Coagulation confined to platelet phospholipids
- Prevents clotting in intact vessels
Phase 3 – Fibrinolysis
- Removes the clot once healing is complete
- Plasminogen → Plasmin → digests fibrin
- Activated by:
- tPA (endothelium)
- Factor XIIa
- Thrombin
- Forms fibrin degradation products:
- E.g. D-dimer – used in clinical tests to assess thrombosis
Summary – Haemostasis
Haemostasis is a highly controlled, three-phase process involving vascular spasm, platelet plug formation, and the coagulation cascade. It halts bleeding, localises clotting to injury sites, and removes clots when no longer needed through fibrinolysis. A clear grasp of this process is vital for diagnosing bleeding or clotting disorders. For a broader context, see our Blood & Haematology Overview page.