Table of Contents
Overview – Haemolytic Disease of Newborn
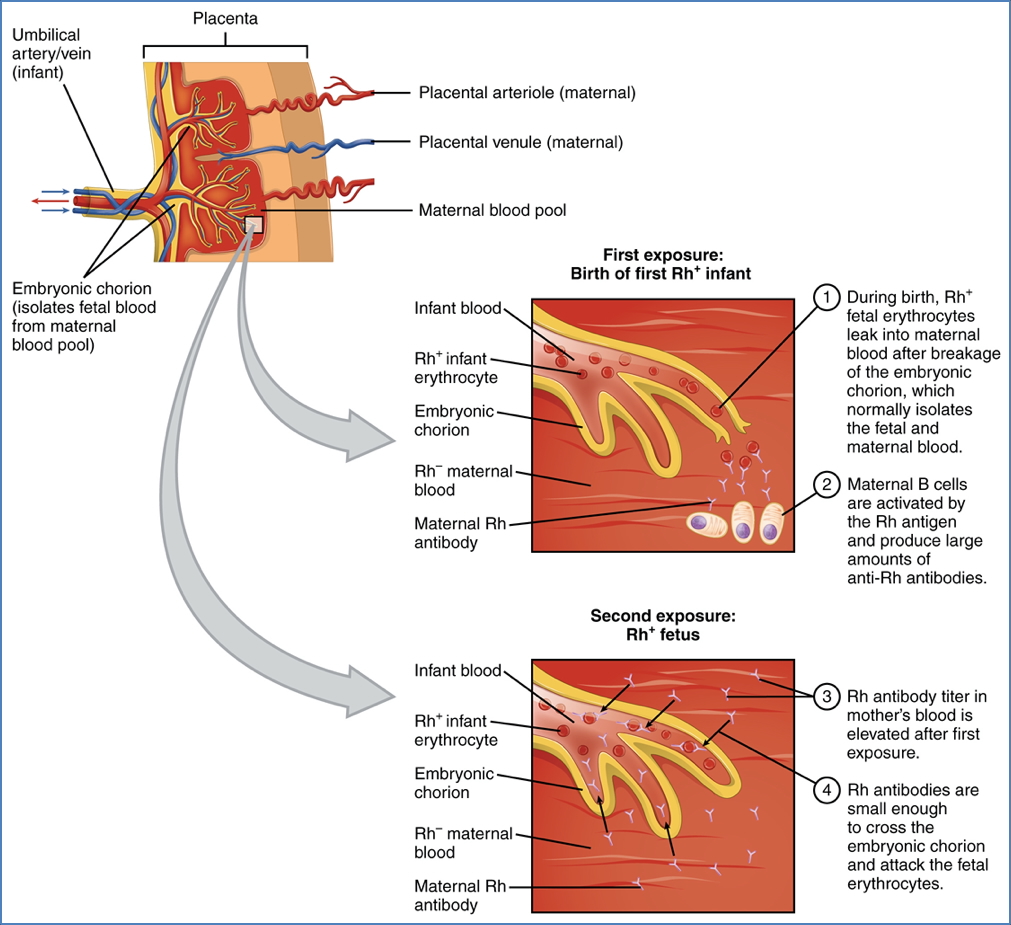
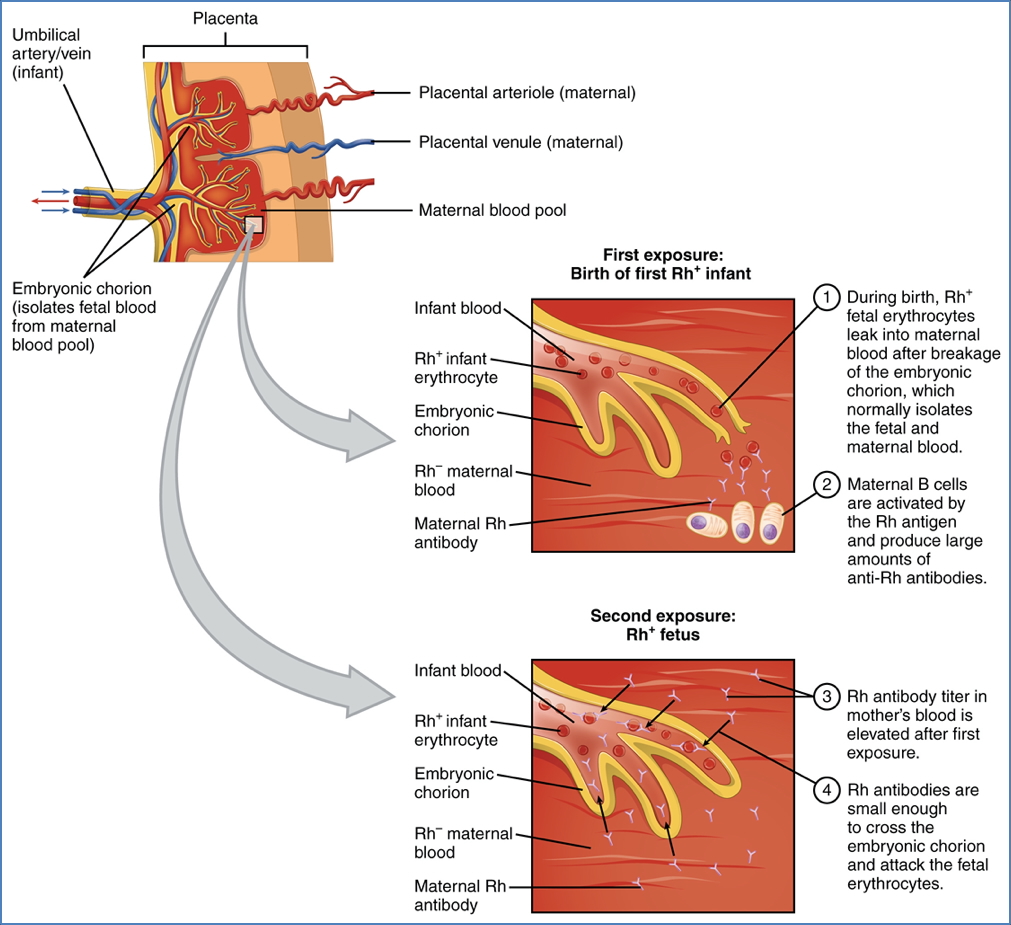
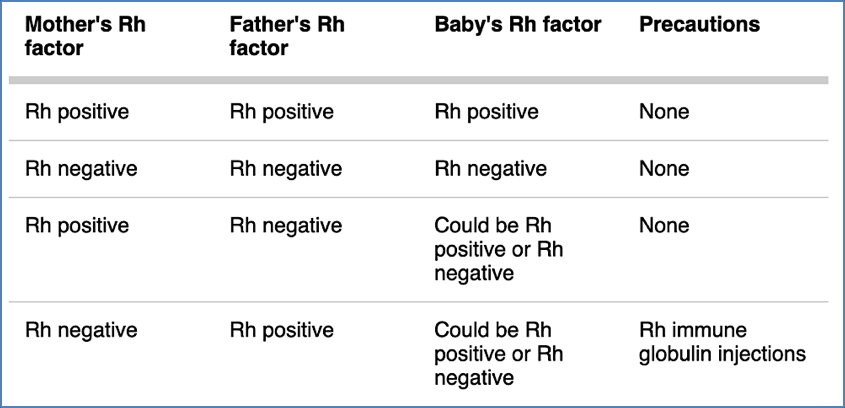
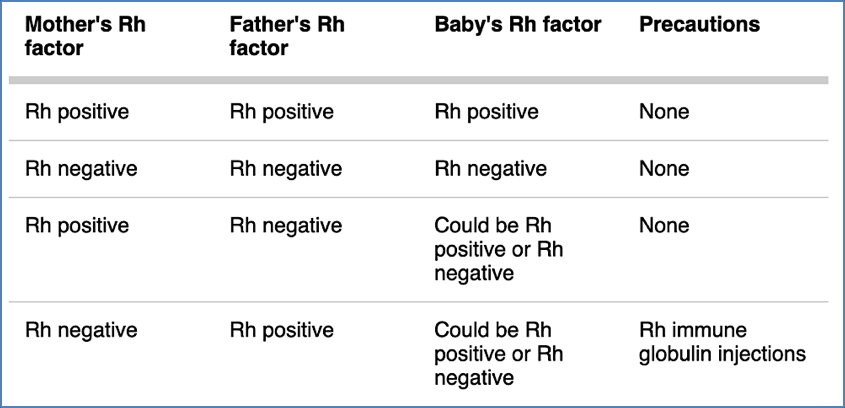
Haemolytic disease of the newborn (HDN) is a serious condition in which maternal IgG antibodies cross the placenta and destroy fetal red blood cells. This immune reaction typically arises when an Rh-negative mother becomes sensitised to Rh-positive fetal blood, leading to antibody-mediated haemolysis in subsequent pregnancies. Without prevention or timely intervention, HDN can cause fetal anaemia, hydrops fetalis, jaundice, or even fetal death. Preventative administration of anti-D immunoglobulin has made this condition largely avoidable in modern obstetrics.
Definition
- Immune-mediated haemolysis of fetal RBCs by maternal IgG antibodies
- Most commonly caused by RhD incompatibility
- Results in fetal anaemia, jaundice, and haemolytic crisis
Pathogenesis
- Mother is RhD-negative (lacks D antigen on her RBCs)
- During pregnancy or delivery, fetal RhD-positive RBCs enter maternal circulation (e.g. via trauma, amniocentesis, or delivery)
- Maternal immune system becomes sensitised, producing anti-D IgG antibodies
- In subsequent pregnancies, these IgG antibodies cross the placenta
- They bind to fetal RhD-positive RBCs → immune-mediated haemolysis
- Haemolysis releases haemoglobin → metabolised to bilirubin, contributing to jaundice
Laboratory Findings
Cord Blood (Fetus)
- RhD positive
- Direct Coombs test: positive (maternal anti-D on fetal RBCs)
- ↑ Bilirubin
- Reticulocytosis from increased erythropoiesis
Maternal Blood
- RhD negative
- Indirect Coombs test: positive (detects maternal anti-D antibodies circulating in plasma)
Clinical Features
- Fetal anaemia
- Hydrops fetalis (in severe cases): ascites, oedema, cardiac failure
- Neonatal jaundice (within first 24–48 hours)
- Hepatosplenomegaly
- Kernicterus (if bilirubin crosses blood-brain barrier)
Prevention
- Anti-D immunoglobulin (passive immunity) given to RhD-negative mothers:
- At 28 weeks’ gestation
- Within 72 hours post-delivery if baby is RhD-positive
- After any sensitising event (e.g. miscarriage, bleeding, procedures)
- The exogenous anti-D binds to fetal RBCs before the maternal immune system is activated
- Prevents primary immune sensitisation
Treatment
- Phototherapy for neonatal jaundice
- Exchange transfusion in severe cases
- Intrauterine transfusion for severe fetal anaemia (detected antenatally)
Summary – Haemolytic Disease of Newborn
Haemolytic disease of the newborn is an immune reaction caused by maternal anti-D antibodies attacking RhD-positive fetal RBCs. It results in fetal anaemia, jaundice, and potentially fatal complications. Prevention through anti-D immunoglobulin administration has dramatically reduced its incidence. For a broader context, see our Blood & Haematology Overview page.