Table of Contents
Overview – Malignant Melanoma
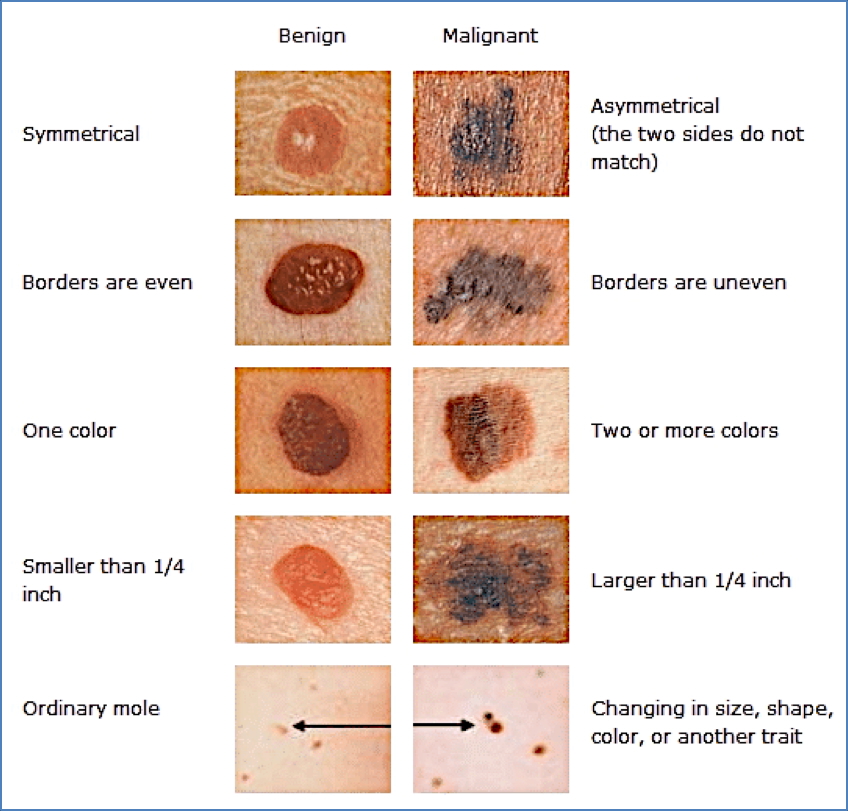
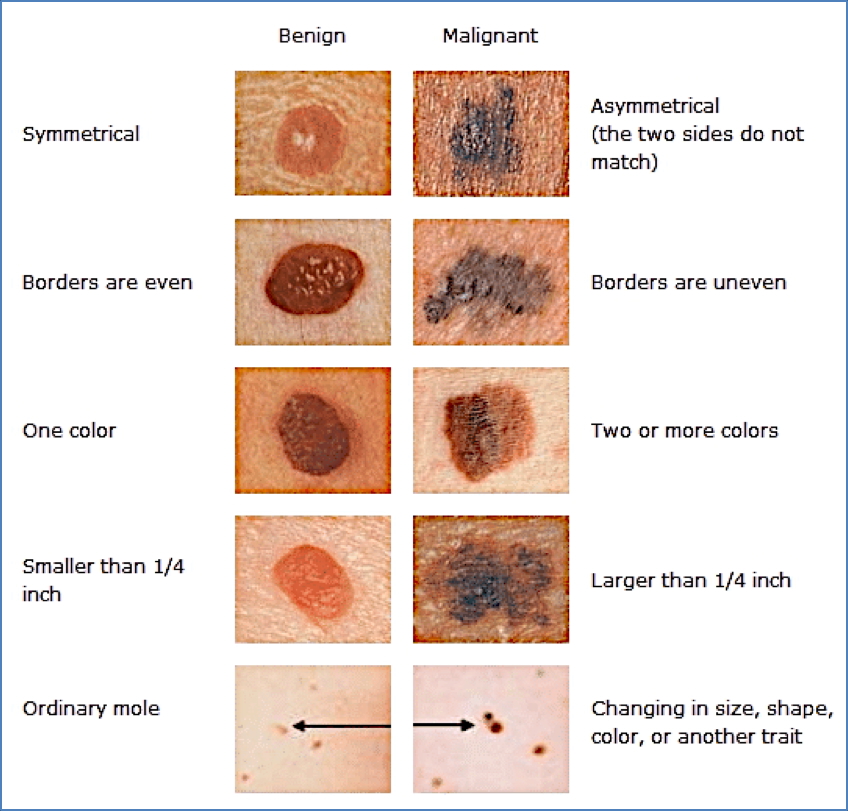
Malignant melanoma is an aggressive skin cancer originating from melanocytes, the pigment-producing cells in the epidermis. It is the third most common cancer in both men and women and is strongly associated with sun exposure, particularly in individuals with fair skin. Early diagnosis and prompt surgical excision are critical, as the prognosis depends heavily on the depth of invasion. Clinicians should remain vigilant for evolving pigmented lesions, particularly those that meet the ABCDE criteria.
Definition
A malignant tumour of melanocytes, typically arising in the skin but also possible in mucosal surfaces or the eye. Known for its potential to metastasize and its association with UV-induced skin damage.
Aetiology
- Chronic and intermittent sun exposure
- Congenital causes (e.g. large congenital naevi)
- Immunosuppression
- Genetic predisposition
Risk Factors
- Family history of melanoma
- Fair complexion, freckles
- Fitzpatrick skin type I/II
- History of severe sunburn, especially in childhood
- High number of common or atypical naevi
- Dysplastic nevus syndrome
- Immunosuppressed states (e.g. transplant recipients)
Pathogenesis
- Tumourigenesis of melanocytes, often beginning in a benign naevus
- Radial Growth Phase (RGP):
→ Lateral expansion with increasing diameter - Vertical Growth Phase (VGP):
→ Downward invasion into dermis; represents more aggressive disease - Common sites: sun-exposed areas, including back, legs, arms, face
Types of Melanoma
- Superficial Spreading Melanoma:
Most common; grows slowly; associated with intermittent sunburn


- Lentigo Maligna Melanoma:
Arises on chronically sun-damaged skin; slow progression


- Nodular Melanoma:
Rapid vertical growth; more aggressive


- Acral Lentiginous Melanoma:
Occurs on palms, soles, nail beds; unrelated to UV; common in darker skin tones


- Amelanotic Melanoma:
Poorly pigmented or red lesions; harder to detect; aggressive behaviour


Morphology
Gross
- Maculopapular lesions
- Irregular shape, colour, and surface
- Often pigmented, but not always (e.g. amelanotic)
Microscopic
- Atypical melanocytes in epidermis and dermis
- Clusters (nests) of abnormal melanocytes
- Mitotic figures present
- Inflammatory infiltrate
- Melanocytes above basal layer (pagetoid spread)
Clinical Features
- Asymmetrical, pigmented lesions with irregular borders
- Itching or bleeding may occur
- Typically a changing mole or new lesion
- Malignant and highly metastatic if not caught early
Diagnosis
- Clinical exam + Dermoscopy (critical)
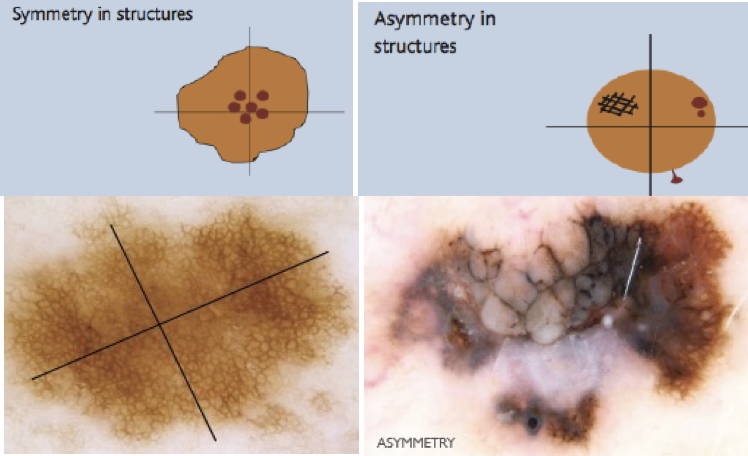
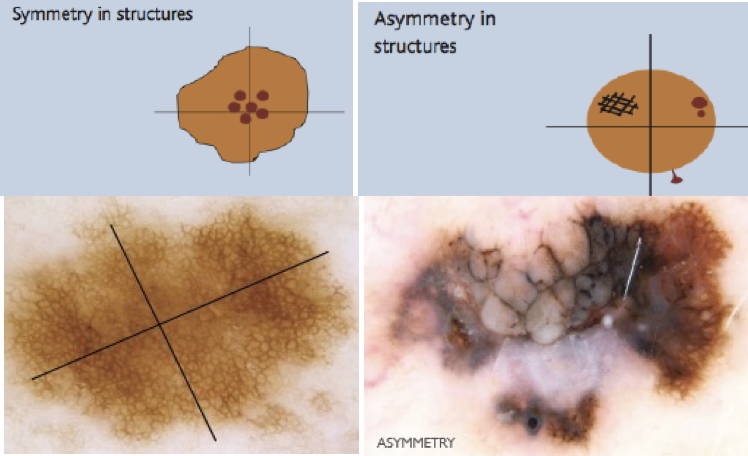
- ABCDE Criteria:
- A: Asymmetry
- B: Border irregularity
- C: Colour variability
- D: Diameter >6mm
- E: Evolving/Elevation/Firm/Growing
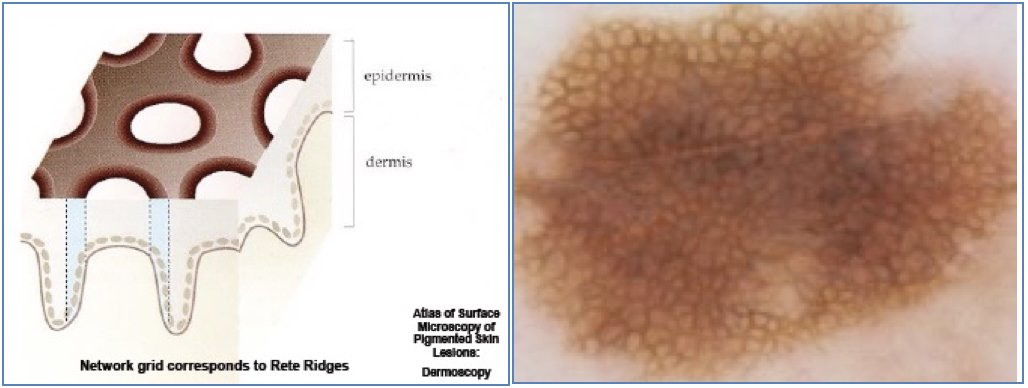
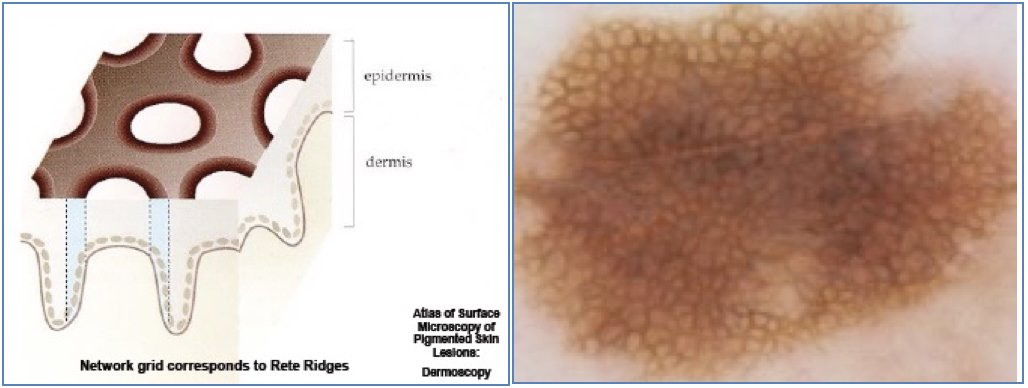
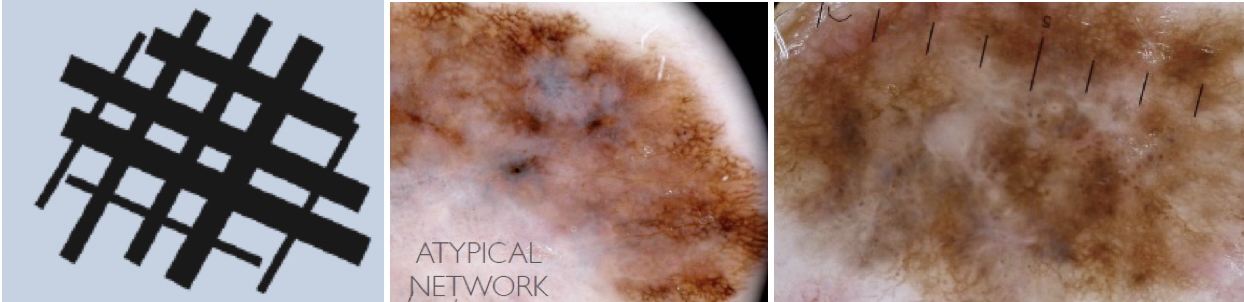
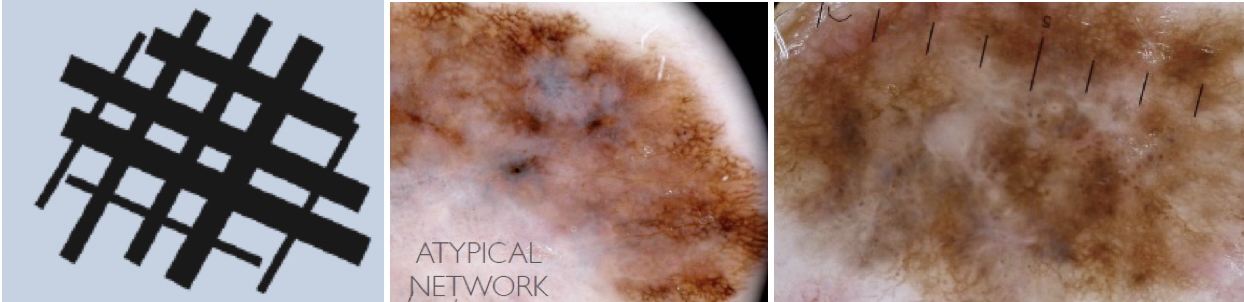
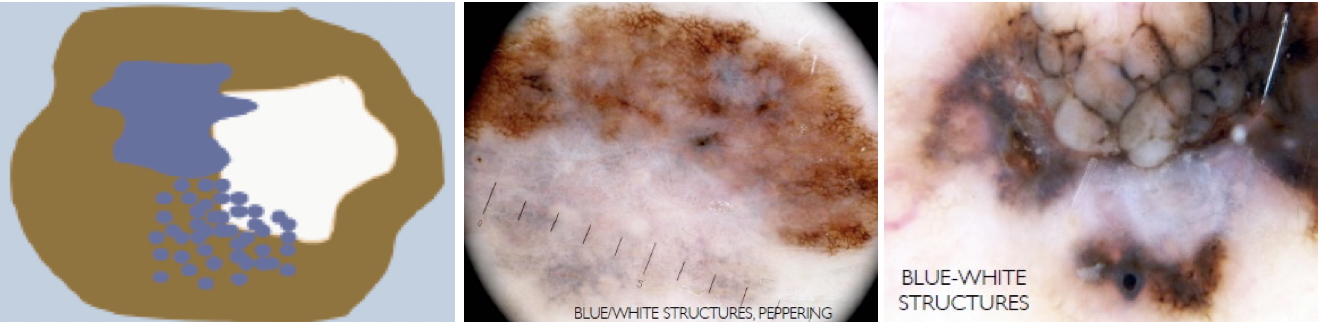
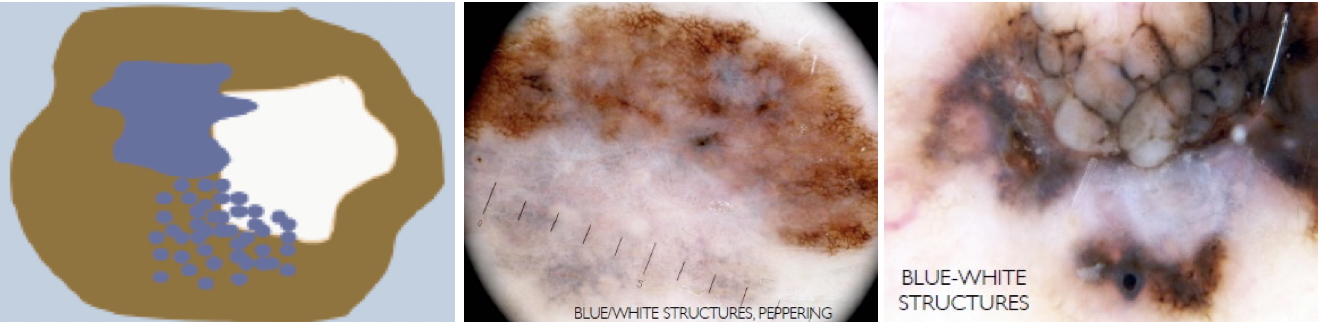
- 3-Point Dermoscopy Checklist (>2 = likely malignant):
- Asymmetry of colour/structure
- Atypical pigment network
- Blue-white structures (peppering, veil, scar)
Prognostic Factors
- Breslow Thickness (most predictive): depth of tumour invasion
- Clark Level: anatomical level of invasion (I–V)
- Ulceration and mitotic rate: indicate poor prognosis
- TNM Staging:
- T = Tumour depth/ulceration
- N = Lymph node involvement
- M = Distant metastases
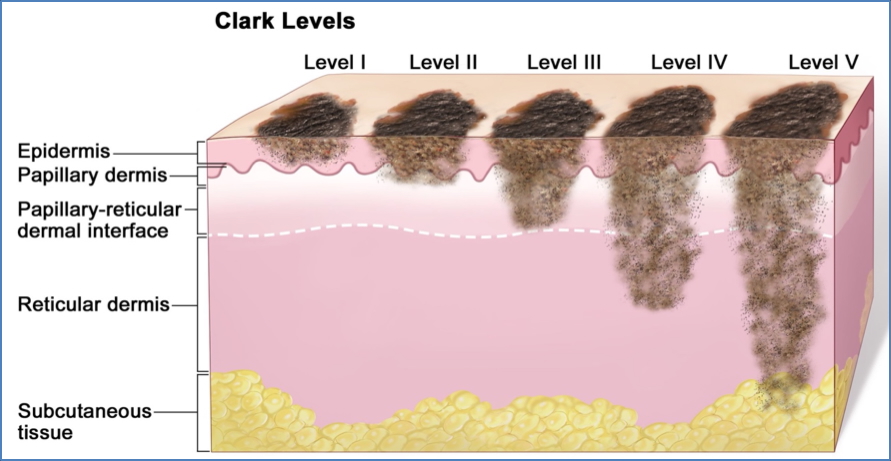
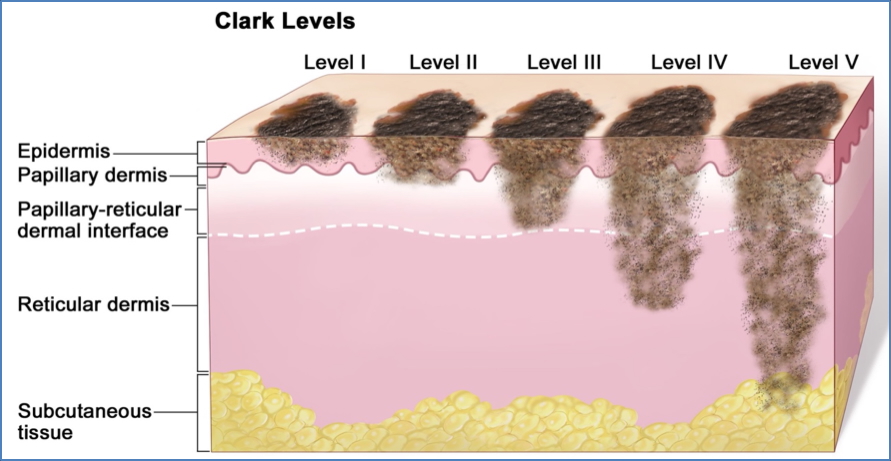
Note: Just realise that despite subtle changes in appearance, the actual size and infiltration of the Melanoma can be quite significant.
Management
- Surgical Excision: Curative if caught early
- Wide local excision margins based on Breslow thickness
- Follow-up: High recurrence risk (13%)
- Adjuvant therapy: For metastatic or high-risk disease
Summary – Malignant Melanoma
Malignant melanoma is a life-threatening skin cancer that arises from melanocytes and often begins in pre-existing naevi. It is diagnosed clinically using dermoscopy and the ABCDE criteria, with prognosis based on Breslow thickness and staging. Early detection and excision are key to survival. For a broader context, see our Skin & Dermatology Overview page.