Table of Contents
Overview – Cellulitis and Erysipelas
Cellulitis and erysipelas are acute bacterial skin infections, frequently seen in general practice, emergency, and paediatric settings. While both conditions involve erythema, swelling, and systemic symptoms, erysipelas is more superficial and sharply demarcated. Differentiating between them is important for targeted antibiotic therapy and managing complications. This topic is essential for medical students and junior doctors.
Definitions
| Condition | Description |
|---|---|
| Cellulitis | Acute bacterial infection of the dermis and subcutaneous tissue |
| Erysipelas | A more superficial bacterial skin infection of the upper dermis and superficial lymphatics |
Aetiology
Cellulitis
- Adults:
- Staphylococcus aureus
- Group A Streptococcus (GAS)
- Children:
- Haemophilus influenzae type B
- Animal bites/scratches:
- Pasteurella multocida (from cats/dogs)
Erysipelas
- Usually caused by:
- Group A Streptococcus (GAS)
- Staphylococcus aureus
- Entry often via breaks in skin (insect bites, ulcers, eczema, fungal infections)
Epidemiology
| Condition | Common Age Group | Common Sites |
|---|---|---|
| Cellulitis | Adults > Children | Lower legs (adults), face (children) |
| Erysipelas | Infants & Elderly | Face, lower limbs |
Pathophysiology
- Skin barrier is breached
- Pathogens invade dermis (and deeper in cellulitis)
- Inflammatory response → oedema, erythema, warmth
- In erysipelas, superficial cutaneous lymphatics are often involved → rapid spread
Clinical Features
Cellulitis
- Painful, diffuse erythema
- Oedema and raised, warm skin
- Possible blistering
- Fever, malaise, regional lymphadenopathy
- Unilateral presentation, usually lower limb
- Risk factors:
- Lymphedema
- Eczema, tinea, HSV
- Trauma, wounds
- Chronic venous insufficiency




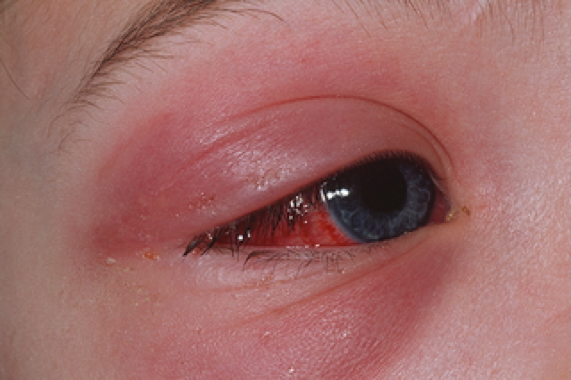
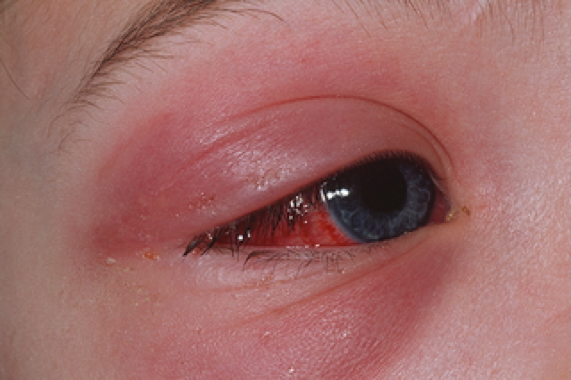
Erysipelas
- More superficial, acute form of cellulitis
- Bright red, firm, and sharply demarcated
- Often described as “St Anthony’s fire” due to burning sensation
- May blister or become necrotic
- Associated with lymphangitis
- Rapid onset of fever and systemic symptoms


Diagnosis
- Clinical diagnosis is typically sufficient
- Swabs or blood cultures if:
- Recurrent infection
- Systemic toxicity
- Immunosuppressed patients
- Ultrasound/CT if abscess suspected
Management
General Measures
- Elevation of affected limb
- Analgesia and hydration
- Treat predisposing conditions
Antibiotic Therapy
- Empiric treatment (mild/moderate):
- Oral penicillins (e.g. flucloxacillin)
- Erythromycin/roxithromycin (if penicillin allergy)
- Severe/systemic symptoms:
- IV penicillins
- Vancomycin (if MRSA suspected)
- Animal bites:
- Amoxicillin-clavulanate
- Orbital cellulitis:
- Immediate hospital admission
- Urgent IV antibiotics
Complications
- Abscess formation
- Necrotising fasciitis
- Sepsis
- Recurrent infections → lymphoedema
- Orbital cellulitis → vision loss, cavernous sinus thrombosis
Summary – Cellulitis and Erysipelas
Cellulitis and erysipelas are acute bacterial skin infections with overlapping features but differing depth and distribution. Cellulitis affects the dermis and subcutaneous tissues and is usually due to Staph aureus or GAS. Erysipelas is a more superficial, sharply demarcated infection caused by GAS. Both require antibiotics and may lead to serious complications if untreated. See our Skin & Dermatology Overview for related topics.