Table of Contents
Overview – Ovarian Tumours
Ovarian tumours include a spectrum from benign cystadenomas to malignant ovarian carcinomas (cystadenocarcinomas) and germ cell-derived teratomas (dermoid cysts). These lesions present diagnostic and therapeutic challenges due to their often asymptomatic nature and high malignancy rates at late stages.
1. Ovarian Cystadenoma (Benign)
Aetiology
- Unknown
Pathogenesis
- Tumour of ovarian surface epithelium
Morphology
- Macro:
- Often large (>20 cm), uni/multiloculated
- Cystic, filled with clear fluid or mucin
- Minimal solid tissue
- Micro:
- Cyst wall lined by cuboidal/columnar epithelium
- May be flat or have small papillary projections
- ± Psammoma bodies (calcifications)
Clinical Features
- Demographics: Common in women aged 20–45
- Symptoms:
- Gradual: abdominal fullness, heaviness
- If ruptured: sudden sharp adnexal pain → radiates to pelvis/back/thighs
- Diagnosis:
- Ultrasound
- CT scan
- Biopsy (definitive)
- Complications:
- Torsion (most common)
- Perforation → acute abdomen
- Infection
Treatment
- Analgesia (paracetamol/NSAIDs)
- COCP to prevent further follicle stimulation
- Non-medical: warm baths, heat packs
- Surgery if large, persistent, or life-threatening
Prognosis
- Benign (~85%)
- Excellent prognosis

2. Ovarian Cancer (Cystadenocarcinoma)
Aetiology
- Unknown
- Risk factors:
- Age >40
- BRCA1/2, HNPCC
- Unopposed estrogen (early menarche, late menopause, nulliparity)
- Smoking, family history
- OCP & multiparity are protective
Pathogenesis
- Carcinogenesis of ovarian serous epithelium
Morphology
- Solid tumour (often with mixed solid-cystic features)
Clinical Features
- Early stages (I–II): usually asymptomatic
- Later stages:
- Pelvic/abdominal pain, bloating, GI/urinary symptoms
- Irregular periods
- Ascites, weight loss, anorexia
- Fixed, solid abdominal/pelvic mass
Diagnosis
- Pelvic exam + transvaginal USS
- CT abdomen/pelvis
- Histology confirms diagnosis
- CA-125 is not for diagnosis – used for monitoring
Treatment
- Surgical debulking
- Intensive chemotherapy
- +/- radiotherapy
Prevention
- Routine screening NOT recommended (due to low sensitivity/specificity of CA-125 and USS)
- High-risk women (e.g. BRCA+, family history):
- Annual screening from age 35 with:
- Pelvic exam
- Transvaginal USS
- CA-125
- Consider prophylactic bilateral salpingo-oophorectomy (BSO)
- +/- mastectomy if BRCA+ due to high breast cancer risk
- Annual screening from age 35 with:
Prognosis
- Malignant (~15%)
- Often diagnosed late → Poor prognosis
- Stage I (ovaries only): 88% 5YS
- Stage II (uterus): 60%
- Stage III (peritoneum): 27%
- Stage IV (distant mets): <10%

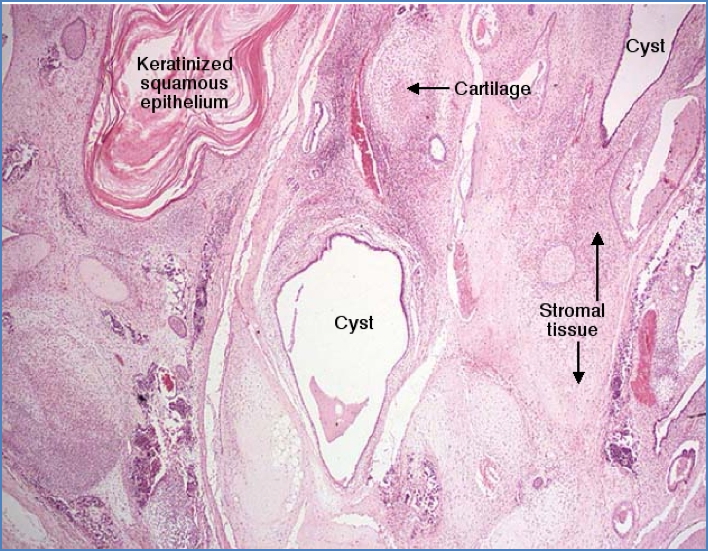
3. Dermoid Cyst (Teratoma)
Aetiology
- Often congenital – slow-growing
- Derived from pluripotent germ cells
Morphology
- Macro:
- May contain hair, teeth, skin, brain, fat, etc.
- Micro:
- Mature tissues from multiple germ layers
- Encapsulated
Clinical Features
- Pelvic/abdominal pain
- Detected via imaging
- Histology confirms
Complications
- Ovarian torsion (especially if large)
- Perforation, haemoperitoneum
- Rare paraneoplastic syndromes:
Treatment
- Surgical removal
Prognosis
- Benign
- Excellent prognosis

2. Unattributable
Summary – Ovarian Tumours
Ovarian tumours can be benign (e.g. cystadenomas, dermoid cysts) or malignant (e.g. cystadenocarcinomas). Symptoms are often vague and diagnosis delayed. Ovarian cancer has poor prognosis due to late detection, but benign tumours typically have excellent outcomes with surgical management. For more resources, visit our Reproductive Health Overview page.