Table of Contents
Overview – Contraception Counselling
Contraception counselling is a structured, patient-centred discussion to explore safe, effective, and acceptable methods of preventing pregnancy. It considers medical history, reproductive goals, personal values, and sexual practices. Effective counselling empowers individuals with informed choices tailored to their unique needs.
Definitions
- Contraception: Prevention of conception (before fertilisation)
- Contragestion: Prevention of pregnancy (after fertilisation)
- Fertility: Ability to conceive and carry a pregnancy to term (≈98% within 12 months in healthy couples)
- Infertility: Failure to conceive after 12 months of regular unprotected sex
- Fecundability: Probability of achieving pregnancy per cycle (~25% in healthy couples)
- Fecundity: Probability of achieving a live birth per cycle
Attributes of an Ideal Contraceptive
- 100% effective
- 100% reversible
- 100% safe (no dangerous/annoying side effects)
- Non-interfering with sexual spontaneity
- Affordable and accessible
- Maintenance-free
- Offers additional benefits (e.g. reduced bleeding, acne control)
Failure Rates
- Expressed as a percentage
- Typical use includes human error
- Perfect use reflects efficacy with exact instructions followed
Types of Contraception
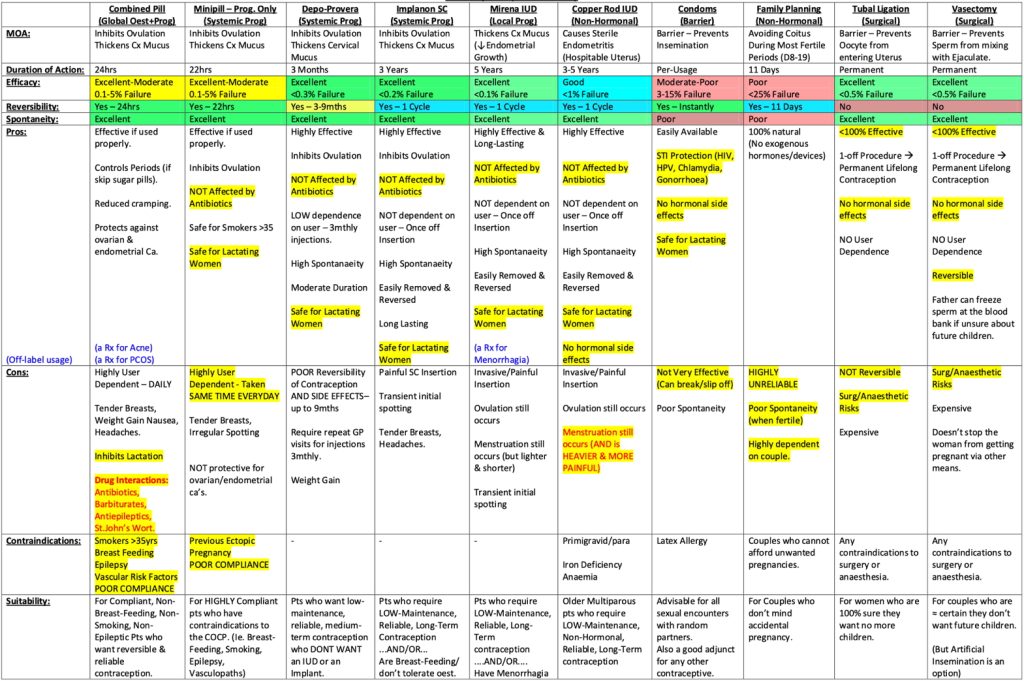
| Method | Description |
|---|---|
| Barrier | Condoms, diaphragms, cervical caps – offer STI protection |
| Hormonal | COCP, POP, implants, injectables, vaginal ring |
| IUCDs | Copper IUD (non-hormonal), Mirena (hormonal) |
| Surgical | Tubal ligation, vasectomy – permanent |
| Behavioural | Withdrawal, periodic abstinence |
| Emergency | Post-coital pills (Plan B) or Copper IUD within 5 days of unprotected sex |
Clinical Interview for Contraception Counselling
A. Assess Goals & Motivations
- Preventing pregnancy?
- Regulating menstruation or treating menorrhagia/dysmenorrhoea?
- STI prevention?
B. Evaluate the Patient’s Context
- Age/Maturity: Tailor approach depending on adolescent vs adult
- Sexual History: Partners, STIs, previous contraception
- Menstrual History: Regularity, dysmenorrhoea, menorrhagia
- Gynaecological/Obstetric Hx: Pap smears, parity, HPV vaccination
- Medical History: Cancer, cardiovascular risk, migraines, diabetes
- Lifestyle: Smoking, drug use, compliance ability
- Consent & Safety: HEADSS screen in <18yo, screen for coercion
Common Contraceptive Options
Combined Oral Contraceptive Pill (COCP)
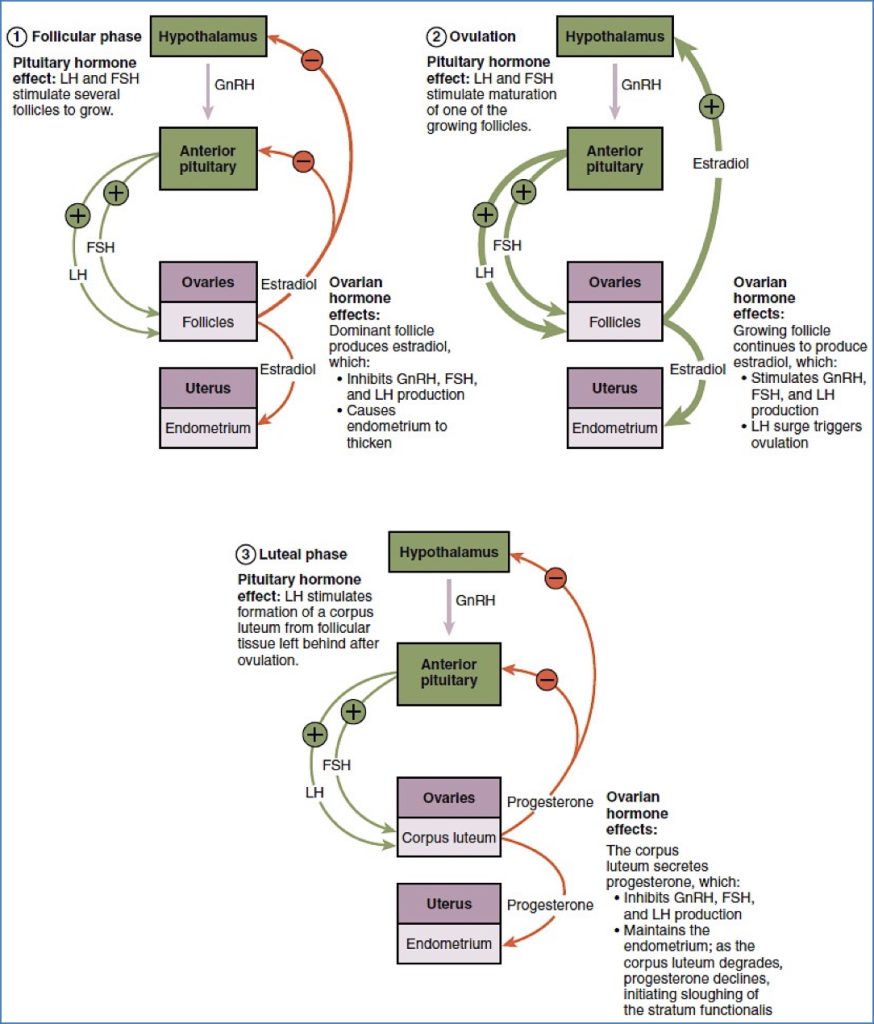
- Inhibits ovulation (↓FSH, ↓LH)
- Improves cycle control, acne, dysmenorrhoea
- Contraindications:
- 35 + smoker
- VTE history, migraines with aura, liver disease
- Side Effects: Headaches, nausea, breast tenderness
- Start: Day 1-5 of cycle + back-up for 7 days
- Missed Pill Management:
- 1 missed: Take ASAP
- 2 missed (Week 1-2): Take 2 today + 2 tomorrow + 7d back-up
- 3 missed: Continue daily + 7d back-up
Progesterone-Only Pill (POP)
- Thickens cervical mucus; partially suppresses ovulation
- Take at the same time daily (3hr window)
- Fewer contraindications (ok for breastfeeding)
- Side Effect: Spotting, irregular bleeding
Depo-Provera (IM Injection)
- Inhibits ovulation, thickens mucus
- Lasts ~3 months
- Start: Day 1-5 of cycle or 6+ weeks postpartum
- Downsides: Weight gain, ↓libido, ↓reversibility (~9 months)
Implanon (Subdermal Rod)
- Effective for 3 years
- Highly reliable; minor compliance needed
- Side Effects: Irregular bleeding, acne, weight changes
Intrauterine Devices (IUDs)
Mirena (Hormonal)
- Local progesterone release → ↓bleeding
- Lasts 5 years
- Bonus: Useful for HRT (progesterone component)
- Side Effects: Irregular bleeding initially
- Contraindications: PID, unexplained bleeding, nulliparity
Copper IUD
- Induces sterile inflammation → Prevents fertilisation
- Lasts 5–10 years
- Bonus: Emergency contraception
- Side Effects: Heavier, crampier periods
Emergency Contraception
- Plan B (Levonorgestrel): Within 72 hrs
- Ulipristal (EllaOne®): Within 120 hrs
- Copper IUD: Most effective within 5 days
Special Populations
| Population | Considerations |
|---|---|
| Adolescents | HEADSS screen; discuss confidentiality & coercion |
| Breastfeeding | Use progesterone-only methods or condoms |
| Postpartum | Avoid COCP <6 weeks; consider POP/Depot/Implanon/Mirena |
| Smokers >35 | Avoid COCP due to VTE risk |
| Chronic Disease | Tailor contraception based on comorbidities |
Case Example – 17-Year-Old Seeking OCP
Assessment:
- History: Sexual activity, STI screen, menstrual irregularity, HEADSS
- Risk screen: Age-gap red flag (25yo partner), consider safety
- Medical: Rule out contraindications (e.g. migraines with aura, smoking)
- STI & Pregnancy Testing
- Discuss safe sex & condom use
- Counsel on COCP side effects & proper use
- Arrange follow-up in 3 months
Summary – Contraception Counselling
- Always assess goals, risks, and preferences
- Emphasise STI protection with hormonal methods
- Provide written instructions for missed pills
- Encourage shared decision-making
- Provide long-term options when appropriate
- Screen for red flags: coercion, abuse, age gaps, unsafe practices
- For a broader context, see our Reproductive Health Overview page.