Table of Contents
Overview – Kidney Fluid Balance
Kidney fluid balance is essential to maintaining homeostasis of electrolytes, plasma osmolality, and blood pressure. Through precise control of water reabsorption, urine concentration, and hormonal signalling, the kidneys ensure that internal fluid volumes are matched to the body’s physiological needs. This topic is foundational for understanding dehydration, oedema, and electrolyte disorders.
Importance of Fluid and Electrolyte Balance
- Essential for normal cell function
- Maintains homeostasis of extracellular fluid
- Supports function of excitable tissues (Na⁺ & K⁺ dependent)
- Integral to blood pressure regulation
Body Fluid Compartments
- Total body water ≈ 40L in adults
- Extracellular fluid (15L)
- Plasma: 3L
- Interstitial fluid: 12L
- Intracellular fluid (25L)
- Extracellular fluid (15L)
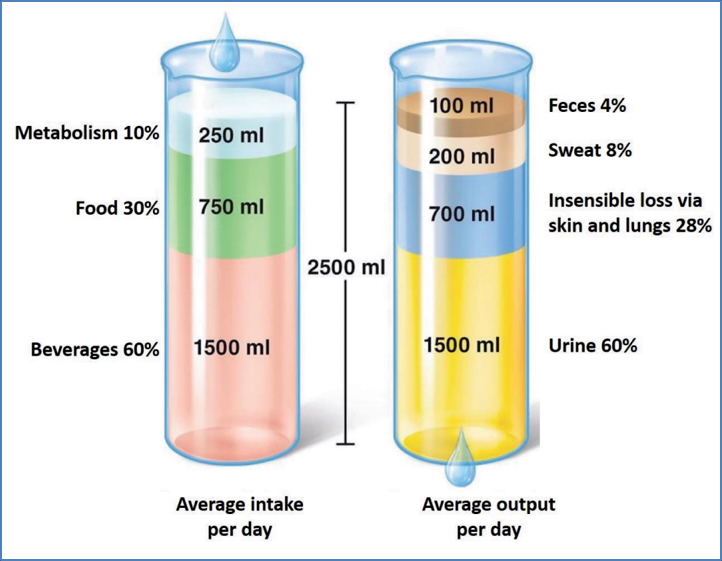
Water Intake and Output
- Intake Sources:
- Metabolism
- Food
- Drinking fluids
- Output Pathways:
- Faeces
- Sweat
- Lungs (insensible loss)
- Urine (primary route of regulation)
Average Daily Balance:
- Intake ≈ 2.5L/day
- Output ≈ 2.5L/day (60% via urine)
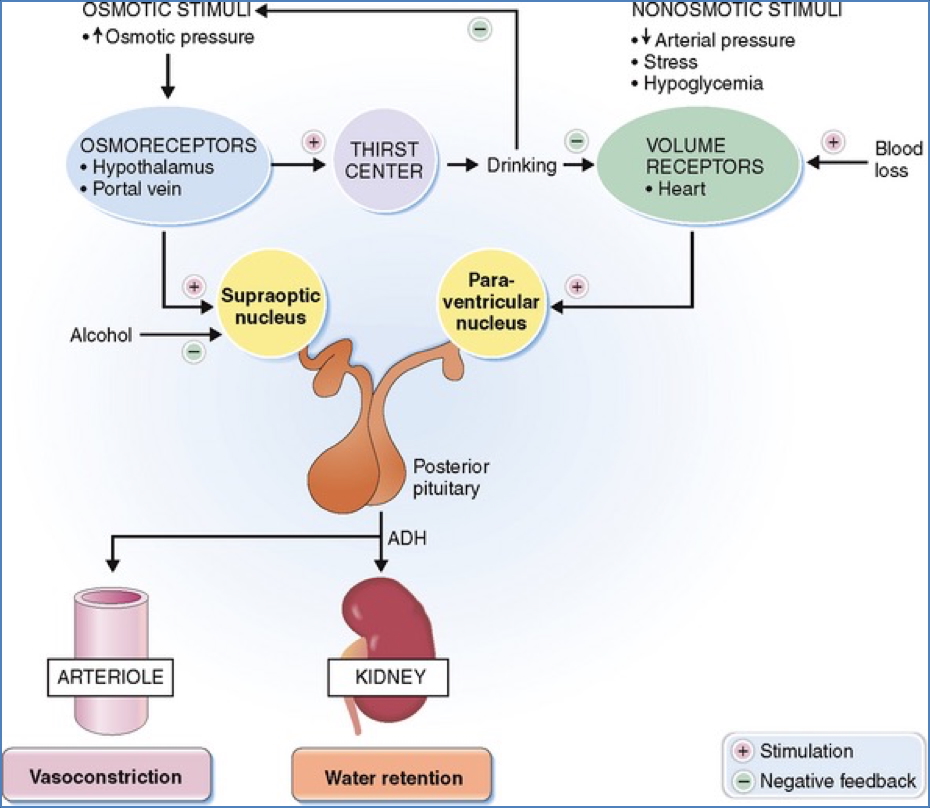
Regulation of Water Intake (Thirst)
Thirst is triggered by:
- ≥10% decrease in plasma volume → reduced salivation → dry mouth → hypothalamic thirst centre activation
- 1–2% increase in plasma osmolality → directly stimulates hypothalamic osmoreceptors
Urine Volume Regulation
- Homeostatic goal: Maintain plasma osmolality at ~300 mOsm
- In water conservation: Low-volume, concentrated urine
- In excess water states: High-volume, dilute urine
Loop of Henle & Counter-Current Multiplication
- Descending limb:
- Permeable to H₂O → passive diffusion into hyperosmotic medulla
- Tubular fluid becomes progressively more concentrated
- Ascending limb:
- Impermeable to H₂O
- Actively pumps Na⁺, Cl⁻ into interstitium → fluid becomes diluted
Vasa Recta (Counter-current exchanger)
- Descending vasa recta:
- Absorbs Na⁺, K⁺, Cl⁻; loses H₂O → becomes hyperosmotic
- Ascending vasa recta:
- Absorbs H₂O; loses solutes → becomes hypo-osmotic
- Maintains medullary osmotic gradient, crucial for water reabsorption

Hormonal Regulation of Fluid Balance
Anti-Diuretic Hormone (ADH / Vasopressin)
- Released from: Posterior pituitary
- Stimulated by:
- Increased plasma osmolality (via osmoreceptors)
- Angiotensin II (in response to renal hypoperfusion)
- Actions:
- Increases H₂O permeability in distal tubule & collecting duct
- Promotes water reabsorption → increases plasma volume, concentrates urine
- Acts synergistically with aldosterone

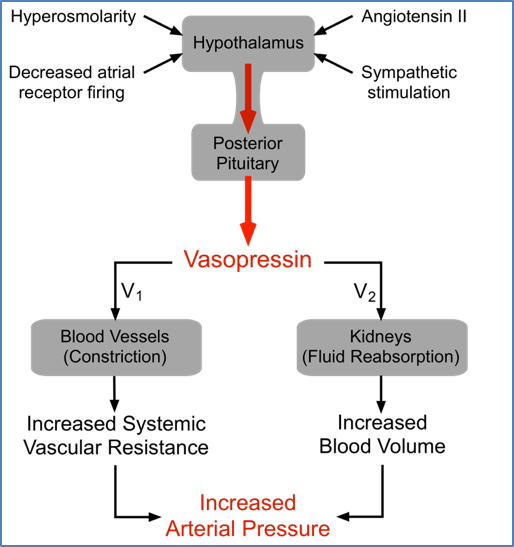
2. Unattributable
3. https://basicmedicalkey.com/the-endocrine-system-7/
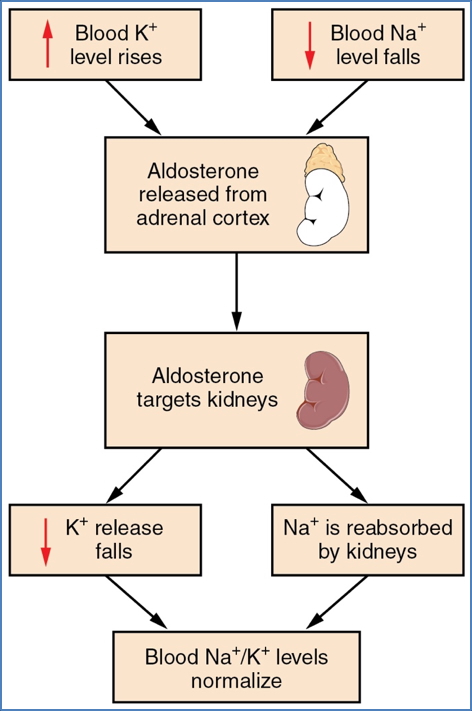
Aldosterone
- Secreted by: Zona glomerulosa of adrenal cortex
- Stimulated by:
- Angiotensin II
- Hyponatraemia
- Hyperkalaemia
- Stress
- Mechanism:
- Activates Na⁺/K⁺-ATPases and ENaC channels
- ↑ Na⁺ & Cl⁻ reabsorption → ↑ extracellular fluid volume
- ↑ K⁺ secretion
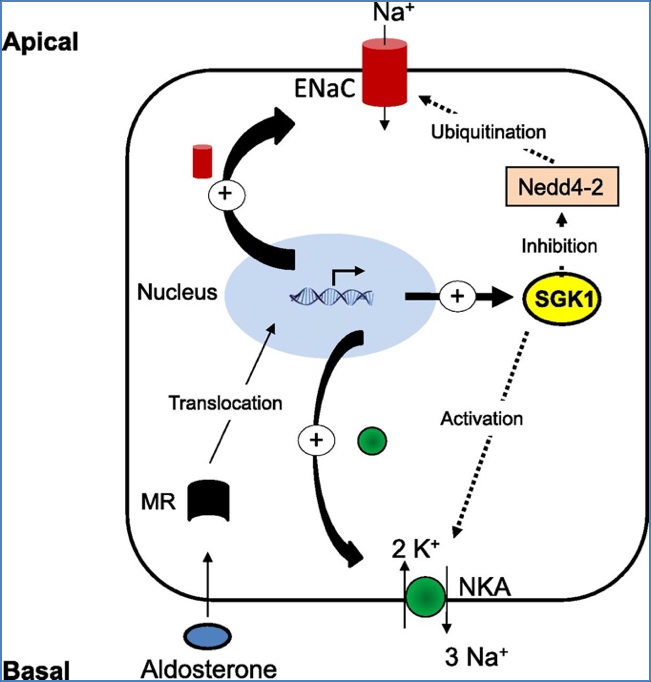
2. OpenStax College, CC BY 3.0 <https://creativecommons.org/licenses/by/3.0>, via Wikimedia Commons
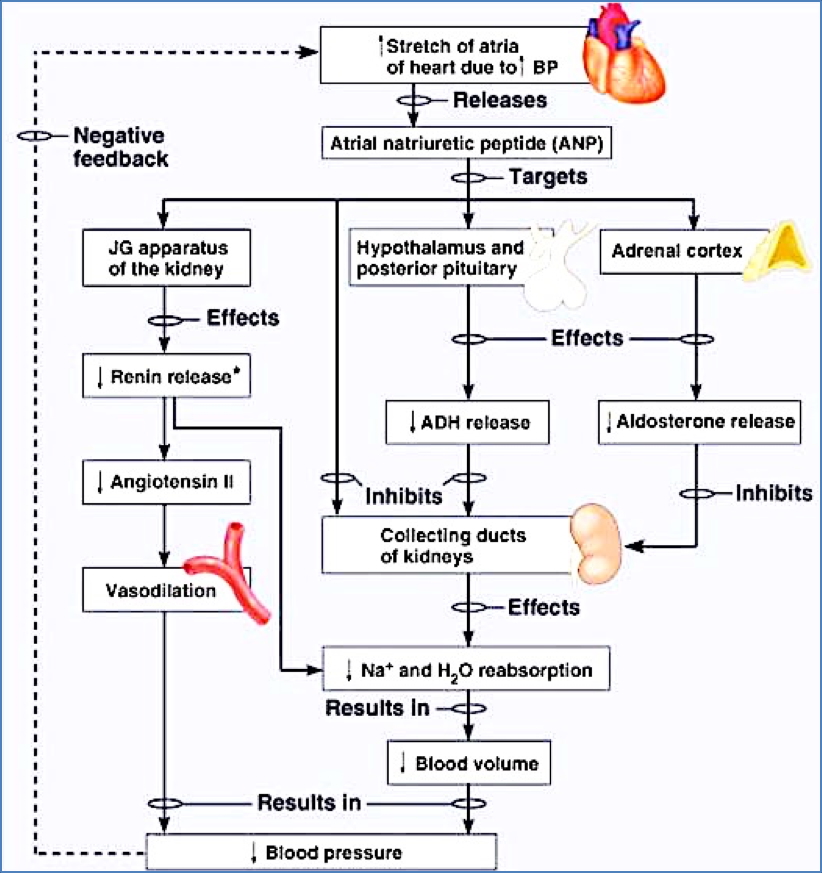
Atrial Natriuretic Peptide (ANP)
- Secreted by: Atrial myocytes
- Triggered by: Atrial stretch (high blood pressure/volume)
- Actions:
- Dilates afferent & constricts efferent arterioles → ↑ GFR
- ↑ Na⁺ & H₂O excretion
- Inhibits renin, aldosterone, and ADH
Summary – Kidney Fluid Balance
Kidney fluid balance is maintained through a coordinated network of water reabsorption, medullary counter-current exchange, and hormone-controlled urine concentration. The kidneys adjust fluid output to maintain plasma osmolality, blood pressure, and electrolyte stability. For a broader context, see our Renal Overview page.