Table of Contents
Overview – Local Anaesthetics
Local anaesthetics are sodium channel-blocking agents used to induce reversible loss of sensation in a specific area without affecting consciousness. These drugs are essential in surgical, dental, and pain-management settings due to their ability to prevent action potential propagation along nerves. Local anaesthetics are widely used across various clinical specialties and routes of administration, and understanding their pharmacodynamics and safe use is vital for final-year medical students.
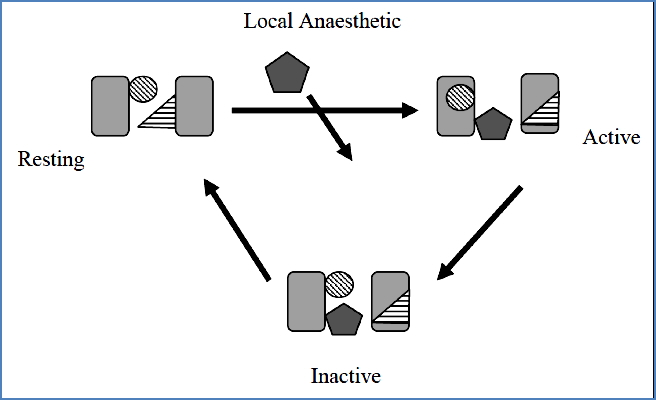
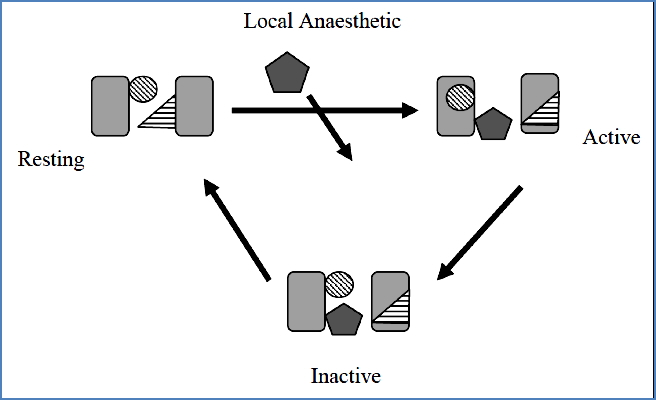
Mechanism of Action
- Voltage-Gated Na⁺ Channel Blockers → Prevent depolarisation → Block action potential propagation
- Affects all types of neurons → Must be administered locally to avoid systemic cardiovascular or CNS effects
- Use-dependent action: Greater effect on rapidly firing neurons (active/inactive channel states only)
- Lipid solubility important for intracellular access to the binding site
- Tissue pH affects ionisation state → Influences lipid solubility & membrane penetration
- Most are weak bases (pKa ~8)
- Acidic environments (e.g. infected tissue) → increased ionisation → ↓effectiveness
Drug Classes & Chemical Properties
- Amide-linked LAs: Preferred for topical anaesthesia
- Rapid onset, prolonged action, higher potency, less vasoconstrictor reliance
- Ester-linked LAs: Less commonly used topically
| Agent | pKa | % Neutral at pH 7.4 | Onset (min) |
|---|---|---|---|
| Bupivacaine | 8.1 | 18% | 5–8 |
| Lignocaine | 7.9 | 25% | 2–4 |
| Procaine | 9.1 | 2% | 14–18 |
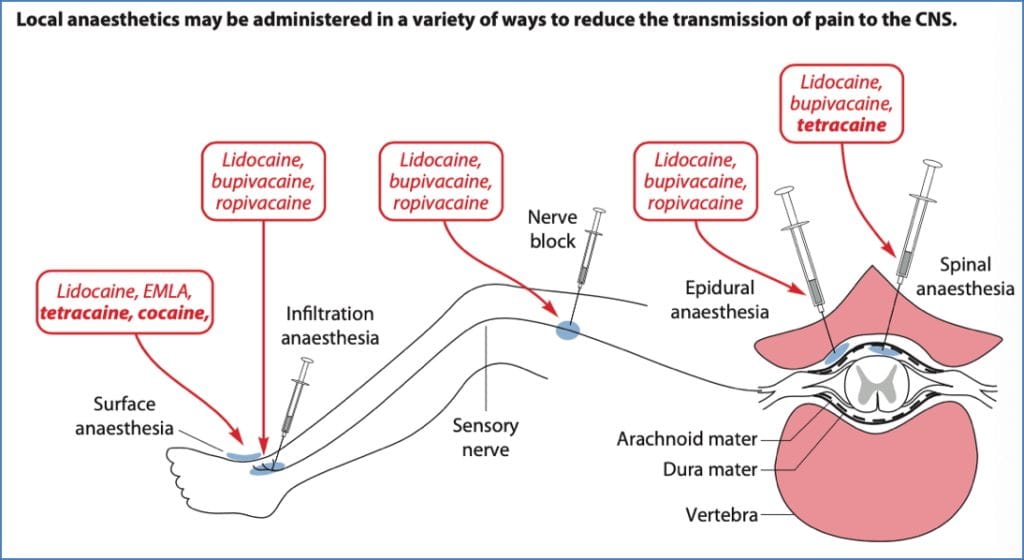
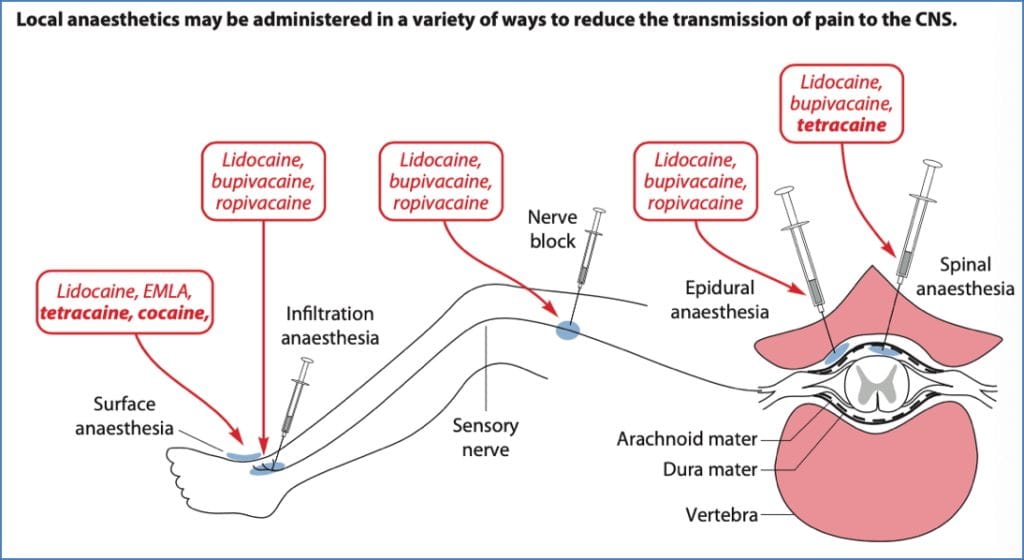
Routes of Administration
Topical Anaesthesia
- Drugs: Tetracaine, Lignocaine, Cocaine
- Features: Creams/ointments; effective on mucous membranes
- Notes:
- Cocaine offers added vasoconstriction
- Adrenaline not useful (can’t penetrate skin)
- ↑Systemic side effects due to rapid absorption
Infiltration Anaesthesia
- Drugs: Lignocaine, Procaine, Bupivacaine
- Direct injection into target tissue
- Adrenaline: Prolongs action but avoid in end-arterial sites (risk of gangrene)
- Pros: Physiological function preserved
- Cons: Large doses needed for small regions
Field Block Anaesthesia
- Subcutaneous injection targeting nerves distal to the injection site
- Used in forearm, scalp, abdomen, limbs
- Pros: Greater coverage with less drug
- Cons: Requires neuroanatomical precision
Nerve Block Anaesthesia
- Injection near peripheral nerves or plexuses
- Pros: Large target area coverage
- Cons: Risk of irreversible nerve damage
Intravenous Regional Anaesthesia (Bier’s Block)
- For limb procedures
- Tourniquet blocks blood flow → LA injected distal to cuff
- Pros: Entire limb coverage
- Cons: Risk of systemic toxicity, ischaemia, pain
Spinal Anaesthesia
- Drugs: Lignocaine, Procaine, Bupivacaine
- Injected into CSF below L2
- Pros: Effective for bowel surgeries (↓peristalsis)
- Cons:
- Vasodilation from sympathetic block
- Hypotension in patients with cardiac compromise
- Risk of cardioacceleratory neuron inhibition
- Post-procedure headaches
Epidural Anaesthesia
- Drugs: Bupivacaine, Etidocaine, Lignocaine
- Injected into epidural space; catheter for continuous delivery
- Pros:
- Safe for labour
- No sympathetic block
- Can co-administer opioids
- Cons:
- Risk of accidental subarachnoid injection
- Higher dose required than spinal → ↑systemic absorption
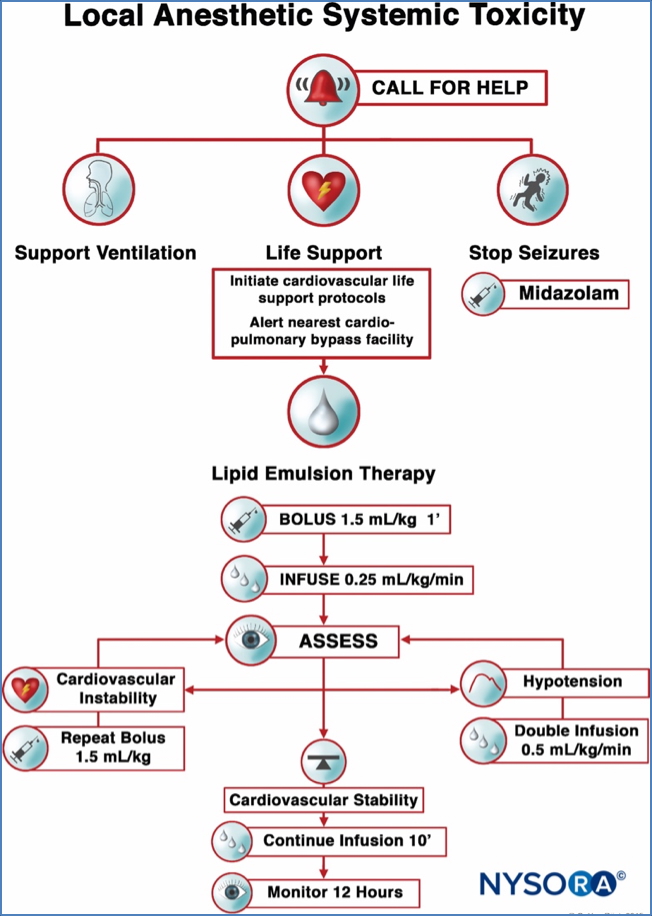
Systemic Side Effects
Most LAs share similar side effects due to shared Na⁺ channel-blocking mechanism
Central Nervous System
- Low–moderate doses → restlessness, tremor, agitation
- High doses → CNS depression, seizures
Cardiovascular & Respiratory
- Respiratory depression
- Cardiac arrhythmias (due to altered myocardial depolarisation)
- ↓Sympathetic tone → hypotension, risk of heart failure in overdose
Muscular Effects
- Neuromuscular blockade at high doses (blocks nicotinic ACh receptors)
- Epidural/spinal → sympathetic paralysis → ↑GI tone
Other Adverse Effects
- Hypersensitivity (dermatitis, rare anaphylaxis)
- Mucosal irritation
Metabolism & Elimination
- Primarily hepatic metabolism
- Transported by plasma proteins; free drug is toxic
- Neonates lack plasma-binding proteins → ↑toxicity risk
Summary – Local Anaesthetics
Local anaesthetics are sodium channel blockers that provide regional anaesthesia by preventing nerve depolarisation. Their effectiveness depends on lipid solubility, use-dependent binding, and tissue pH. Routes of administration vary widely, each with unique benefits and risks. Systemic toxicity remains a concern, especially in vulnerable populations like neonates or during high-dose use. For more foundational principles, visit our Pharmacology & Toxicology Overview page.