Table of Contents
Overview – Antipsychotic Drugs
Antipsychotic drugs are the cornerstone of treatment for psychosis, including schizophrenia, where patients experience delusions, hallucinations, or disorganised thought. These drugs primarily work by antagonising dopamine D2-like receptors in key central nervous system pathways. Understanding their mechanisms, classifications, and side effects is crucial for safe and effective management of psychiatric disorders.
Definition
- Psychosis: A mental state involving a loss of contact with reality, often characterised by delusions, hallucinations, or thought disturbances.
- Schizophrenia: A group of chronic psychotic disorders with phases of acute symptoms and functional decline.
- Positive symptoms: Hallucinations, delusions, disorganised speech and behaviour
- Negative symptoms: Blunted affect, poor motivation, cognitive impairment
Aetiology
- Unknown exact cause
- Involves dysfunction in dopaminergic pathways, especially:
- Mesolimbic system
- Nigrostriatal pathway
- Dopamine is the primary neurotransmitter implicated
- Additional contributors:
- Genetic: e.g. COMT gene; 10% increased risk with first-degree relative
- Environmental: prenatal infections, psychosocial stressors
- Other neurotransmitters: glutamate, serotonin, GABA
Pathophysiology
1. Dopamine Hypothesis
- Psychosis results from overactivity of dopaminergic pathways (↑ dopamine or ↑ D2 receptors)
- Explains positive symptoms, but not negative symptoms
- Incomplete model (e.g. treatment delay, other transmitter involvement)
2. Dysregulation Hypothesis
- Broadens dopamine theory
- Dysfunction across multiple pathways due to:
- Receptor number/sensitivity changes
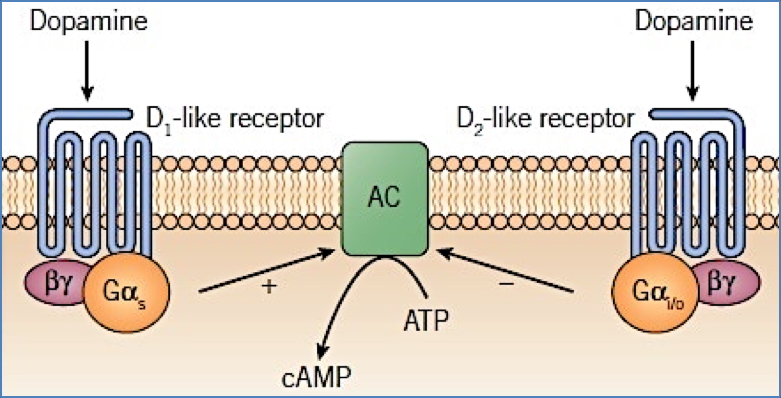
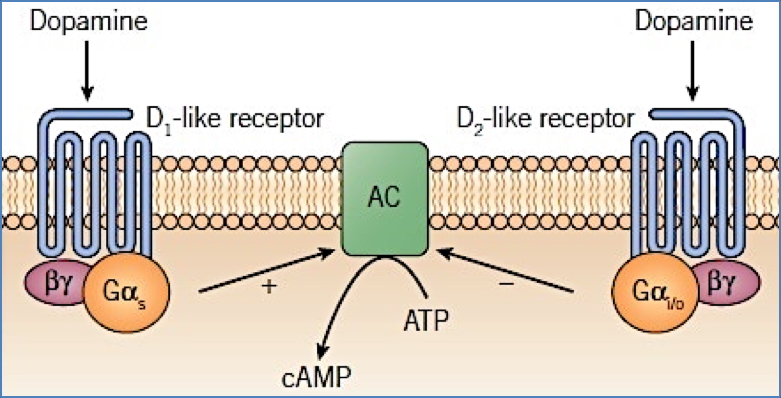
- Signalling cascade dysfunction (via adenylate cyclase)
- Altered neurotransmitter synthesis/metabolism/reuptake
- Involves glutamate (NMDA-R), serotonin (5HT), GABA
Dopamine Pathways & Clinical Effects
| Pathway | Role | Blockade Effects |
|---|---|---|
| Mesolimbic | Reward, psychosis | ↓ positive symptoms (therapeutic target) |
| Nigrostriatal | Movement | Extrapyramidal side effects |
| Tuberoinfundibular | Hormone regulation | ↑ prolactin secretion |
| Medullary-periventricular | Appetite, behaviour | Weight changes |
Mechanism of Action
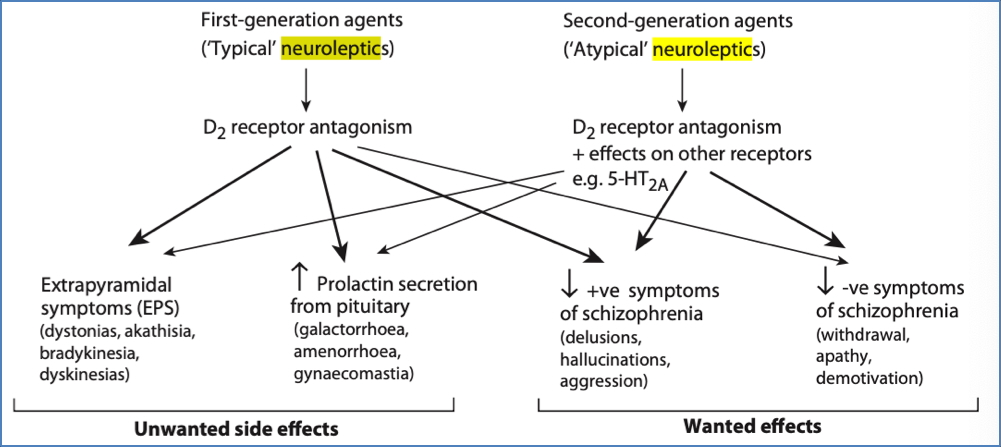
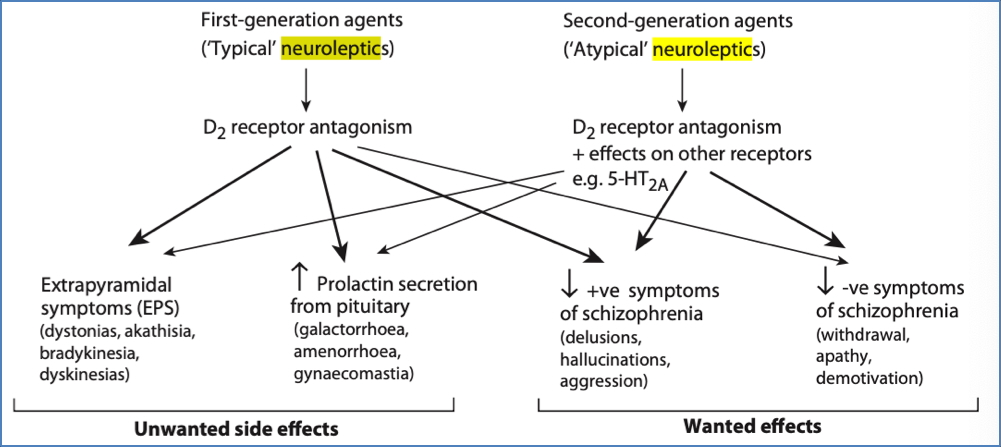
- Antipsychotics = neuroleptics
- Primarily D2-like receptor antagonists → ↓ adenylate cyclase activity
- Some drugs also affect:
- D4 receptors
- 5HT receptors (particularly in atypicals)
Drug Classes
1. Based on Side Effect Profile
| Type | Motor Side Effects | Main Receptor Action | Examples |
|---|---|---|---|
| Typical | Yes (extrapyramidal) | D2 antagonists (non-selective) | Chlorpromazine, Haloperidol |
| Atypical | Minimal | D2 + 5HT2A antagonists, selective D4 | Clozapine, Olanzapine, Sulpiride |
2. Based on Structure
- Phenothiazines: Chlorpromazine, Fluphenazine, Trifluoperazine
- Heterocyclics: Haloperidol, Risperidone, Clozapine, Olanzapine
Side Effects
1. Motor (Extrapyramidal)
- Akathisia – restlessness
- Pseudoparkinsonism – tremor, rigidity
- Dystonia – facial/neck spasms
- Tardive dyskinesia – repetitive movements (face, trunk, limbs)
2. Endocrine
- ↑ Prolactin → menstrual changes, gynecomastia, galactorrhoea, ↓ libido
3. Antimuscarinic
- Dry mouth, blurred vision, tachycardia, constipation, urinary retention
4. Anti-adrenergic
- Hypotension (α₁-blockade)
5. Antihistaminergic
- Sedation
- Weight gain (often significant)
6. Hypersensitivity & Rare Effects
- Obstructive jaundice
- Agranulocytosis (especially clozapine)
- Neuroleptic Malignant Syndrome (rare, potentially fatal): hyperthermia + rigidity
Neuroplasticity & Treatment Lag
- Why do antipsychotics take 2–3 weeks to work?
- Believed to trigger remodelling (like long-term potentiation)
- Involves changes in:
- Receptor number and subtype
- G-protein coupling
- Intracellular signalling and enzyme profiles


Compliance Considerations
- Compliance is often poor due to:
- Delayed onset of therapeutic effect
- Paranoia and mistrust
- Disruption of perceived ‘benefits’ (e.g. creativity)
- Poor time awareness
- Long-acting injectable depot forms are useful alternatives
Summary – Antipsychotic Drugs
Antipsychotic drugs work primarily by blocking dopamine D2 receptors in the mesolimbic system to reduce psychotic symptoms. They are classified as typical or atypical based on their side effect profiles, particularly motor effects. Their full therapeutic action is often delayed due to synaptic remodelling. For a broader pharmacological context, see our Pharmacology & Toxicology Overview page.