Table of Contents
Overview – Antihypertensive Drugs
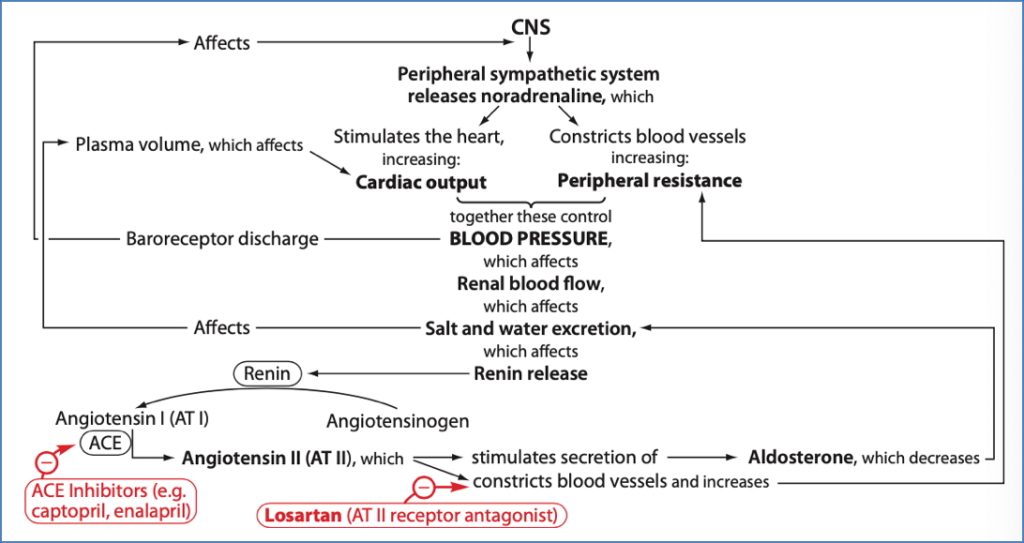
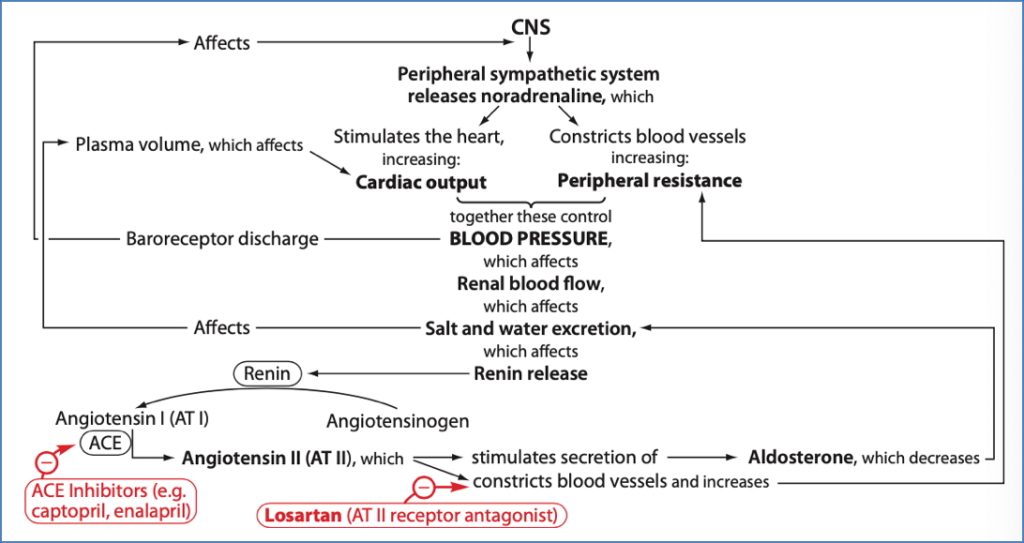
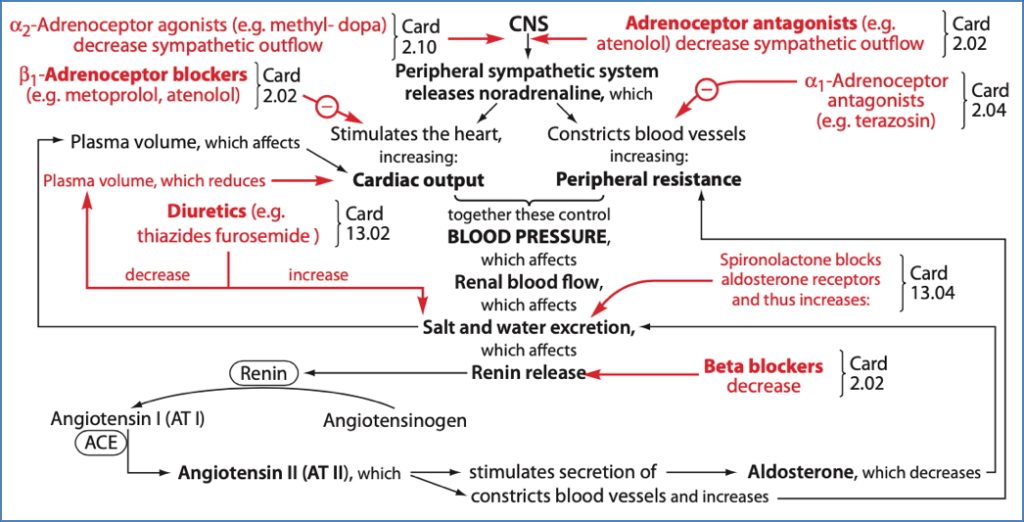
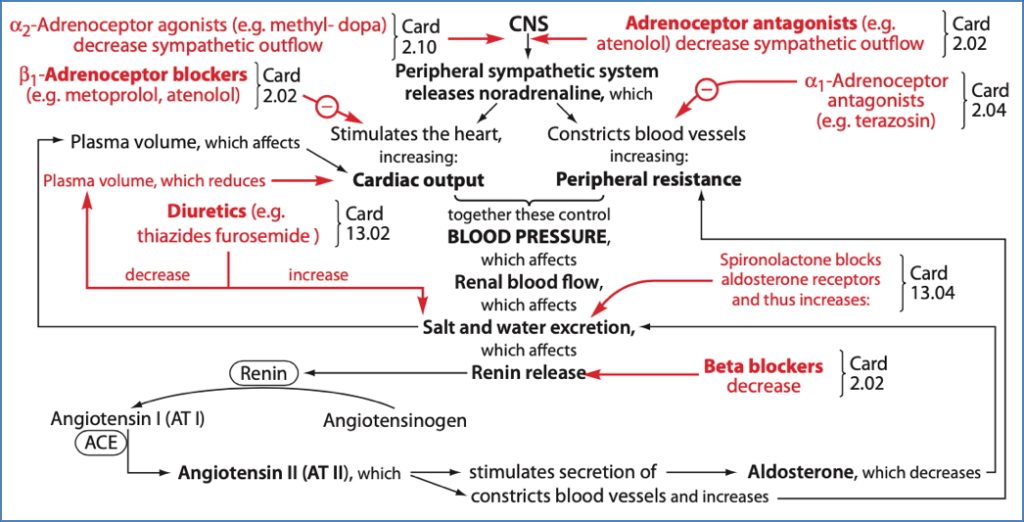
Antihypertensive drugs are a cornerstone of cardiovascular disease prevention, especially in patients with long-term risks such as diabetes, kidney disease, or prior myocardial infarction. These medications work by reducing systemic vascular resistance, cardiac output, or both. First-line choices depend on patient age, ethnicity, comorbidities, and renin profile. This page outlines the core pharmacological classes of antihypertensives, their mechanisms, clinical indications, and key side effects.
Therapeutic Approach to Hypertension
Non-Pharmacological Management
- Lifestyle changes are first-line:
- Increased physical activity and dietary fibre
- Reduced salt and saturated fat intake
- Weight reduction
Pharmacological Strategy
- Step 1: Start with either an ACE inhibitor or angiotensin-II receptor blocker (ARB)
- Preferred for younger or white patients (high-renin profile)
- Step 2: Add a thiazide diuretic or calcium channel blocker
- Especially effective in elderly or Afro-Caribbean patients (low-renin profile)
- Adjunct options:
- β-blockers: Useful in patients with concurrent angina or heart failure
- α-blockers: Considered in males with coexistent prostatic hypertrophy (watch for postural hypotension)
ACE Inhibitors (“-prils”)
Mechanism of Action
- Inhibit angiotensin-converting enzyme (ACE) → ↓ Angiotensin-II production
- ↓ Vasoconstriction → Vasodilation
- ↓ Aldosterone secretion → ↓ Na⁺ & water retention
- ↓ ADH release and sympathetic activity
- Overall → ↓ Blood pressure
Indications
- Hypertension
- Congestive heart failure
- Post-myocardial infarction
- Ischaemic heart disease prevention
- Diabetic nephropathy
- Renal insufficiency (Caution: contraindicated in severe renal artery stenosis)
Common Agents
- Captopril, Enalapril, Ramipril, Perindopril, Trandolapril
Side Effects
- Dry cough (common)
- Hypotension
- Hyperkalaemia (due to ↓ aldosterone)
Angiotensin-II Receptor Blockers (ARBs) (“-sartans”)
Mechanism of Action
- Directly block angiotensin-II receptors on vascular smooth muscle
- ↓ Vasoconstriction, aldosterone, ADH, and sympathetic outflow
- Overall → ↓ Blood pressure
Indications
- Hypertension (especially in diabetics or younger patients)
- Heart failure
- Diabetic nephropathy
Common Agents
- Valsartan, Losartan, Candesartan, Irbesartan
Side Effects
- Hypotension
- Hyperkalaemia
- No dry cough (unlike ACE inhibitors)
Beta-Blockers (“-olols”)
Mechanism of Action
- Inhibit β1-adrenoceptors on cardiac muscle →:
- ↓ Heart rate and contractility → ↓ cardiac output
- ↓ Renin release → ↓ angiotensin-II, aldosterone, ADH
- ↓ Sympathetic activity
Indications
- Hypertension
- Angina
- Secondary prevention post-myocardial infarction
Common Agents
- Atenolol, Oxprenolol
Side Effects
- Bronchoconstriction (caution in asthma/COPD)
- Bradycardia, potential heart block
- Cold extremities
- Fatigue
Alpha-Blockers (“-osins”)
Mechanism of Action
- Block α1-adrenoceptors on vascular smooth muscle → vasodilation
- Also relax bladder neck and prostate → improved urine flow
Indications
- Resistant hypertension
- Benign prostatic hyperplasia (BPH)
Common Agents
- Prazosin, Tamsulosin
Side Effects
- Postural hypotension (may cause dizziness or syncope)
- Insomnia
- Priapism
- Abnormal ejaculation
Summary – Antihypertensive Drugs
Antihypertensive drugs are essential in the long-term prevention of cardiovascular disease. Key classes include ACE inhibitors, angiotensin receptor blockers, beta-blockers, and alpha-blockers — each with distinct mechanisms, indications, and adverse effect profiles. Choosing the right antihypertensive requires tailoring to patient age, comorbidities, and renin status. For a broader context, see our Pharmacology & Toxicology Overview page.