Table of Contents
Overview – Preterm Labour
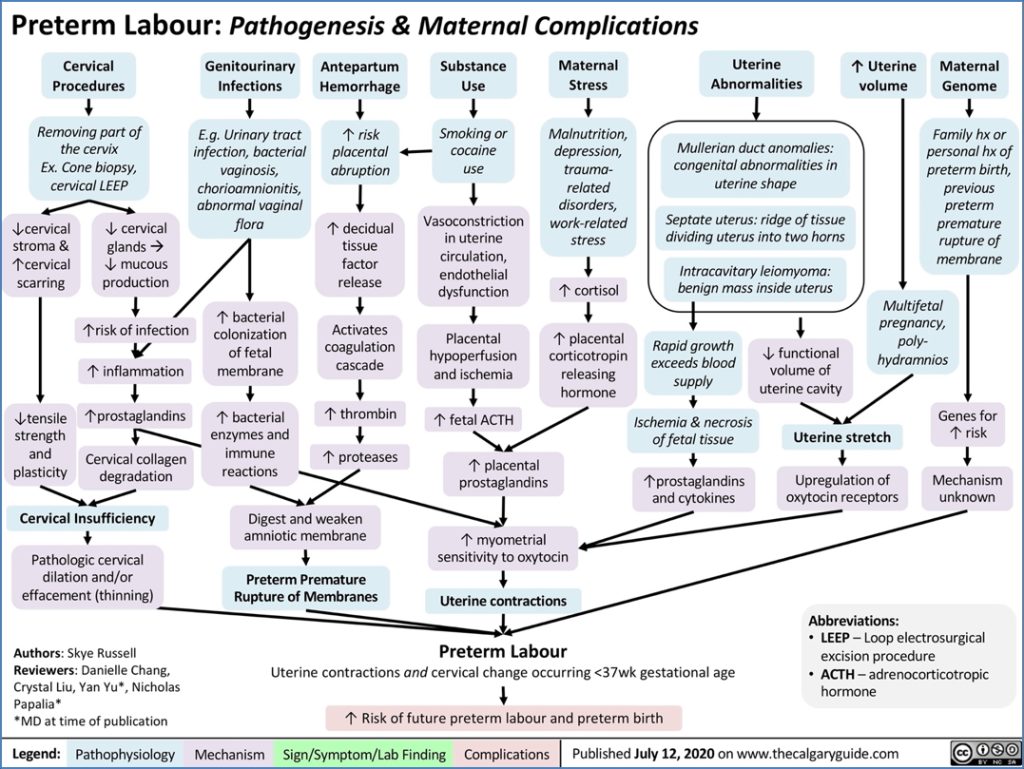
Preterm labour refers to the onset of labour between 20 and 37 weeks of gestation. It is a leading cause of neonatal morbidity and mortality, accounting for around 10% of all pregnancies. While the majority of cases are idiopathic, several maternal, fetal, and uterine factors can contribute. Timely recognition and appropriate management are critical for improving neonatal outcomes.
Definition
- Onset of labour (regular contractions + cervical changes) between 20 and 37 weeks gestation.
Aetiology
Most cases are idiopathic, but potential triggers include:
Maternal Factors
- Infection
- Hypertension
- Diabetes
- Trauma or injury
- Poor nutrition
- Substance use (alcohol, smoking, recreational drugs)
Placental Causes
- Preterm premature rupture of membranes (PPROM)
- Placenta previa
- Placental abruption
- Placental insufficiency
Fetal Factors
- Multiple gestation
- Congenital anomalies
- Fetal stress
- Hydrops fetalis
Uterine Factors
- Uterine malformations (e.g. Müllerian anomalies)
- Leiomyomas (fibroids)
Epidemiology
- Occurs in approximately 10% of pregnancies.
Risk Factors
- Previous preterm labour
- Prior cervical cone biopsy or mechanical dilation
- Short cervical length on transvaginal ultrasound (TVUS)
- Cervical length >30mm = lower risk
- Advanced maternal age
- Smoking
- Multiple pregnancies
Clinical Features
- Regular uterine contractions
- Cervical effacement and dilation between 20–37 weeks gestation
Investigations
- Transvaginal ultrasound (TVUS): Assess cervical length
- Fetal ultrasound: Evaluate fetal growth, position, and placental location
- Fetal fibronectin test: Can help assess risk of preterm birth in symptomatic women
- Urine MCS, CRP, full blood count (FBC): Rule out infection
- CTG (cardiotocography): Fetal well-being
Management
Initial Measures
- Admit to birthing unit or hospital
- Hydration
- Bed rest, preferably in left lateral position
- Fetal ultrasound for presentation and placental evaluation
Tocolysis (Labour Suppression)
- Goal: Delay delivery to allow corticosteroids to mature fetal lungs
- Eligibility Criteria:
- Live, immature fetus
- Intact membranes
- Cervical dilation <4 cm
- Contraindications:
- Maternal: Active bleeding, preeclampsia/eclampsia, chorioamnionitis
- Fetal: Intrauterine growth restriction (IUGR), fetal distress or demise
Pharmacologic Agents
- Nifedipine (calcium channel blocker) – first-line tocolytic
- Indomethacin (prostaglandin synthesis inhibitor)
- Magnesium sulfate – for eclampsia prophylaxis, and may offer fetal neuroprotection
- Betamethasone – accelerates fetal lung maturity
Prognosis
- Survival outcomes improve with advancing gestation and weight:
- 30 weeks / >1500g → ~90% survival
- 33 weeks / >2000g → ~99% survival

Complications
- Neonatal respiratory distress syndrome
- Sepsis
- Intraventricular hemorrhage
- Necrotizing enterocolitis
- Long-term neurodevelopmental delay
- Maternal stress and delivery-related complications
Differential Diagnosis
- Braxton-Hicks contractions
- Urinary tract infection
- Placental abruption
- Cervical incompetence
- Acute chorioamnionitis
Summary – Preterm Labour
Preterm labour refers to the onset of uterine contractions and cervical dilation between 20 and 37 weeks gestation. It affects around 10% of pregnancies and can result from maternal, fetal, placental, or uterine factors. Management focuses on identifying those at risk, delaying delivery when appropriate, and optimising fetal outcomes through corticosteroids and supportive care. For a broader context, see our Obstetrics Overview page.