Table of Contents
Overview – Public Health Overview
Public health overview refers to the organised efforts and informed choices of society, communities, and individuals to promote health, prevent disease, and prolong life. This page explores key definitions, prevention strategies, screening principles, and landmark successes that define modern public health and population health strategies—knowledge crucial for final-year medical students navigating both clinical and community contexts.
Definition
- Population Health
Focuses on the health outcomes of specific groups, influenced by:- Physical, biological, social, environmental, and economic factors
- Personal health behaviours
- Availability and accessibility of health services
- Public Health
Societal programs and policies aimed at:- Protecting and restoring health
- Preventing morbidity and mortality
- Implemented through practices, policies, programs, and institutions
- Epidemiology
The study of disease distribution and determinants in populations - Preventative Medicine
A medical discipline targeting risk factors to minimise disease manifestation - Aetiology (Etiology)
The study of causes and contributing factors of diseases - Risk Factor
Any attribute that increases disease likelihood, including:- Demographic, behavioural, biomedical, genetic, environmental, and social factors
Goals of Public Health Services
- Health Protection – e.g. water safety, food regulation
- Surveillance – early detection of epidemics or harmful behaviours
- Disease and Injury Prevention – e.g. vaccination, PPE mandates
- Population Assessment – community needs evaluation
- Health Promotion – community engagement, policy, and interventions
- Preparedness and Response – planning for pandemics, disasters, etc.
Concepts of Health
- Wellness – dynamic well-being across physical, mental, social, and spiritual domains
- Disease – medically defined structural or functional abnormality
- Illness – individual’s subjective perception of unwellness
- Sickness – societal perception and behavioural response to illness
- Impairment – structural/functional loss or abnormality
- Disability – restrictions in performing typical human activities
Disease Burden Metrics
- DALY (Disability-Adjusted Life Years) – total years lost due to illness/disability + early death
- YLL (Years of Life Lost) – due to premature mortality
- YLD (Years Lived with Disability) – time spent with health conditions


Why Prevent Disease?
- Improves patient outcomes
- Reduces disability and mortality
- Prevents incurable diseases (e.g. HIV/AIDS)
- Cost-effective – 70% of GP visits are chronic disease-related
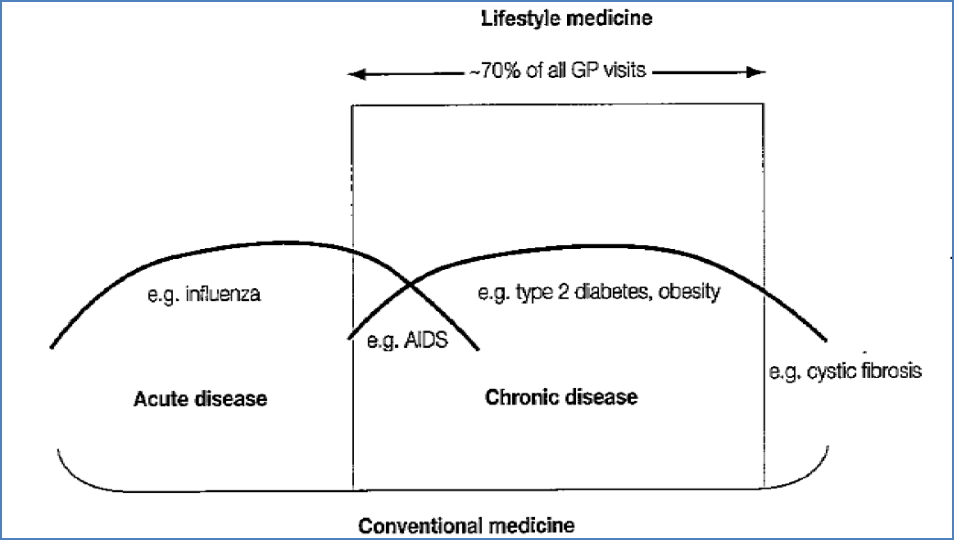
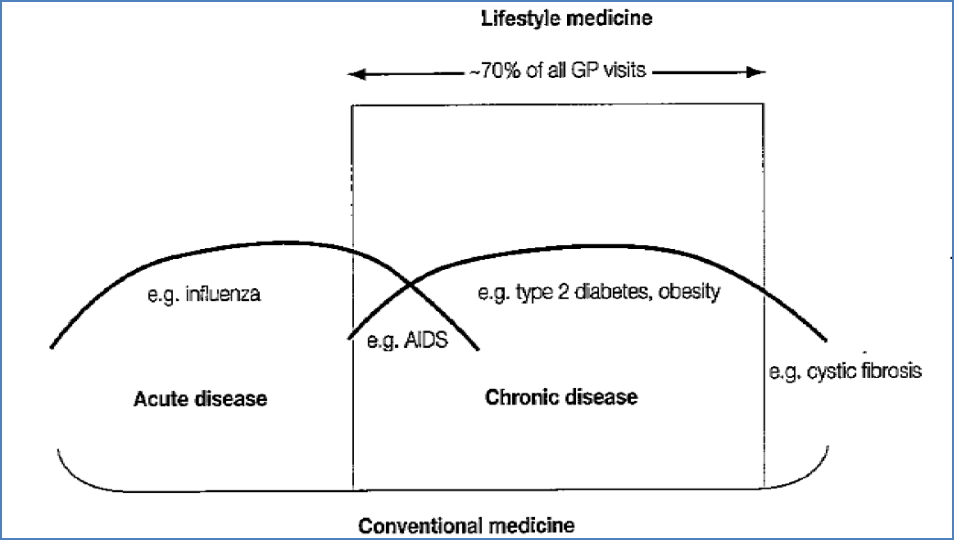
Types of Prevention
- Primary Prevention – Prevent disease onset
- Eg: Immunisation, dietary changes, seat belts
- Secondary Prevention – Detect early and intervene
- Eg: Hypertension screening, mammography, Pap smears
- Tertiary Prevention – Reduce complications of established disease
- Eg: Bariatric surgery, diabetes management, long-term medications
Screening Principles
Screening aims to identify individuals more likely to benefit than be harmed by further tests or treatments.
Criteria for Screening:
- Disease must have significant burden
- Detectable early (latent) stage or identifiable risk factors
- Tests must be simple, safe, validated, and acceptable
- Effective treatment must be available
- Early treatment must improve prognosis (mortality, morbidity, quality of life)
Prevention Strategies
1. High-Risk Strategy
- Targets individuals at elevated risk
- Methods: Opportunistic screening, medical intervention
- Pros: Tailored, cost-effective
- Cons: Screening complexities, predictive limitations, resource-heavy
2. Population Strategy
- Shifts entire population’s exposure level
- Methods: Policy, behavioural/environmental change
- Pros: Small changes = large population impact
- Cons: Low personal motivation, limited individual benefit


Common Disease Prevention Practices
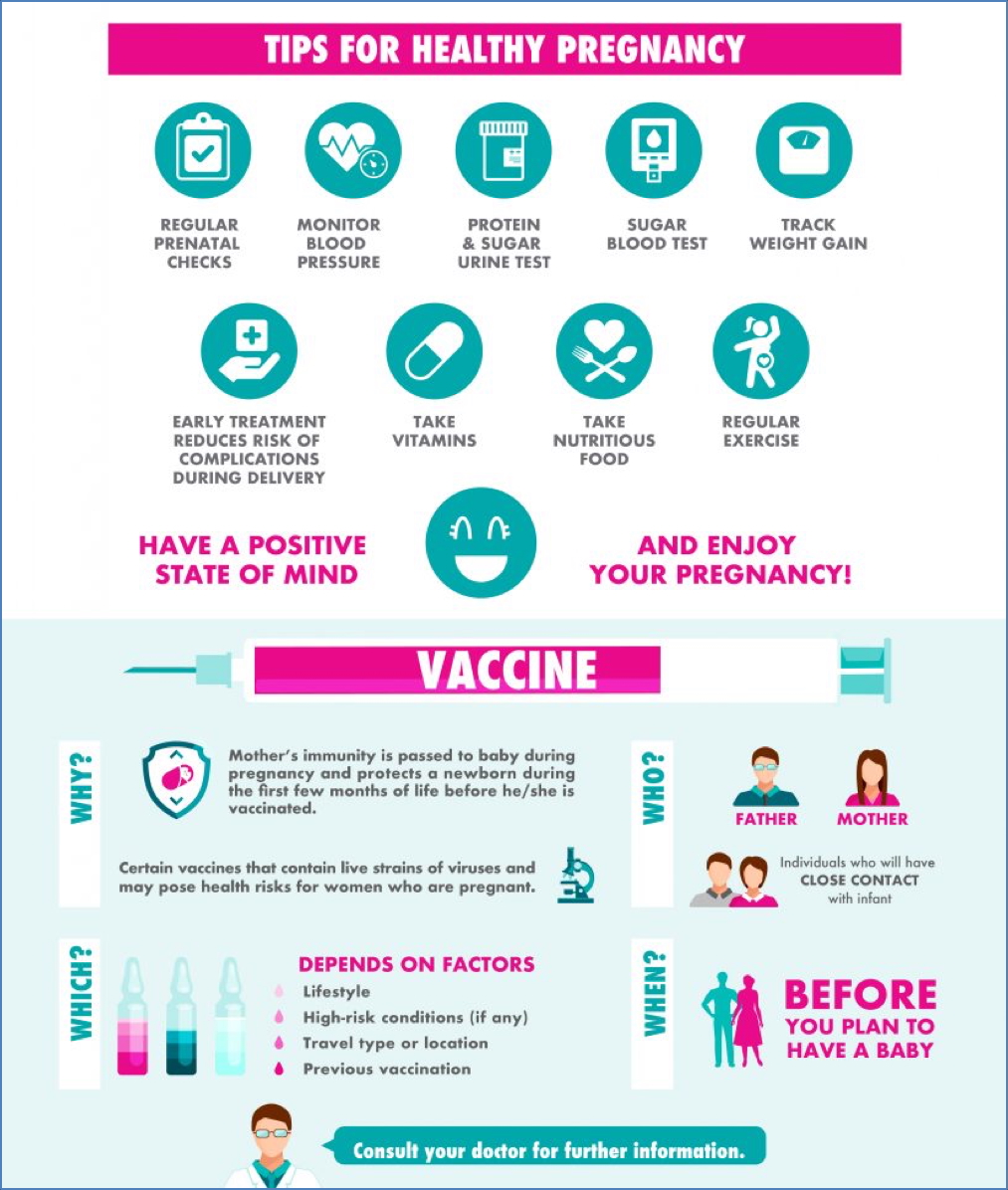
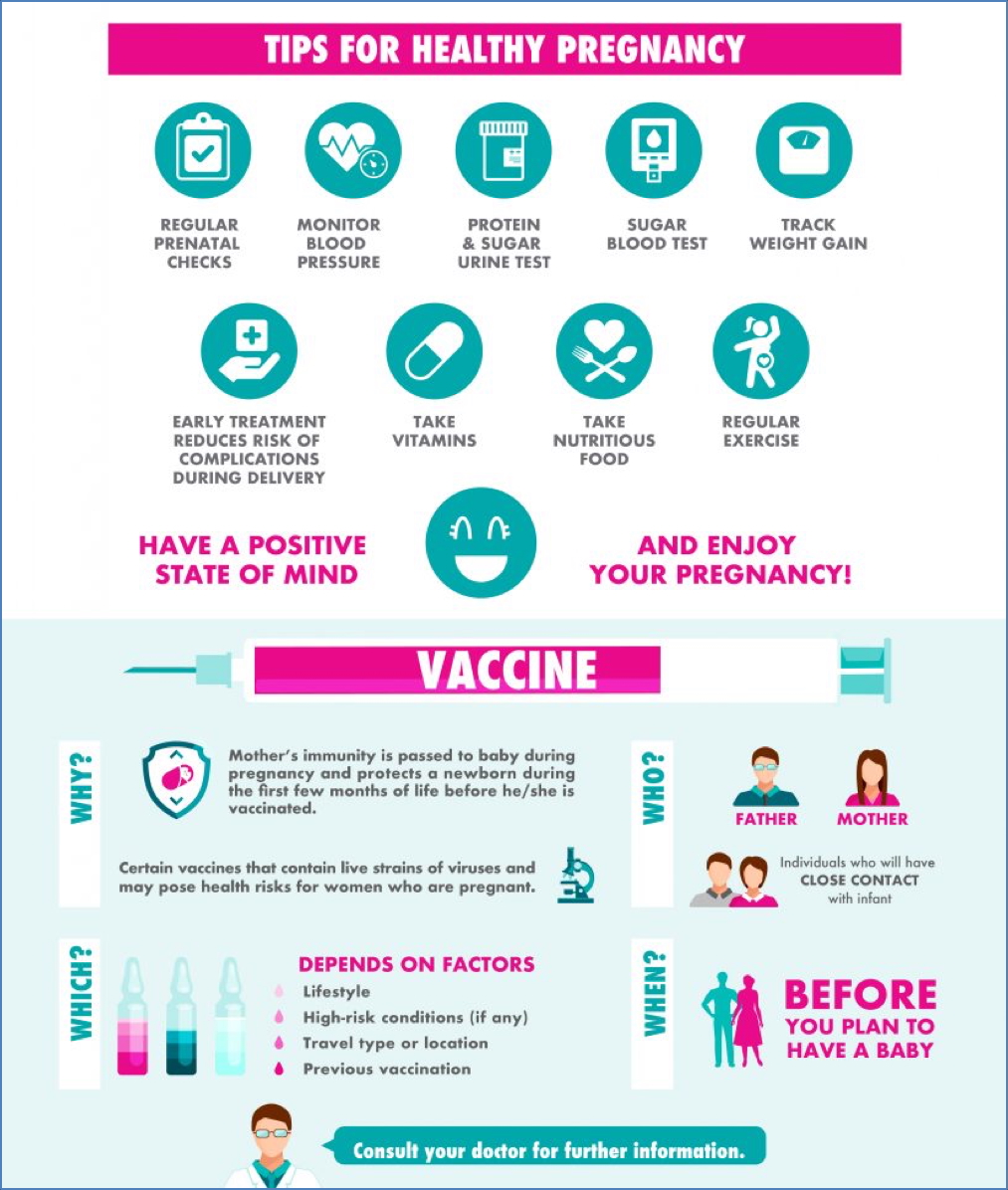
- Pregnancy: Folate, Rubella immunity, genetic testing, hygiene, no alcohol/smoking
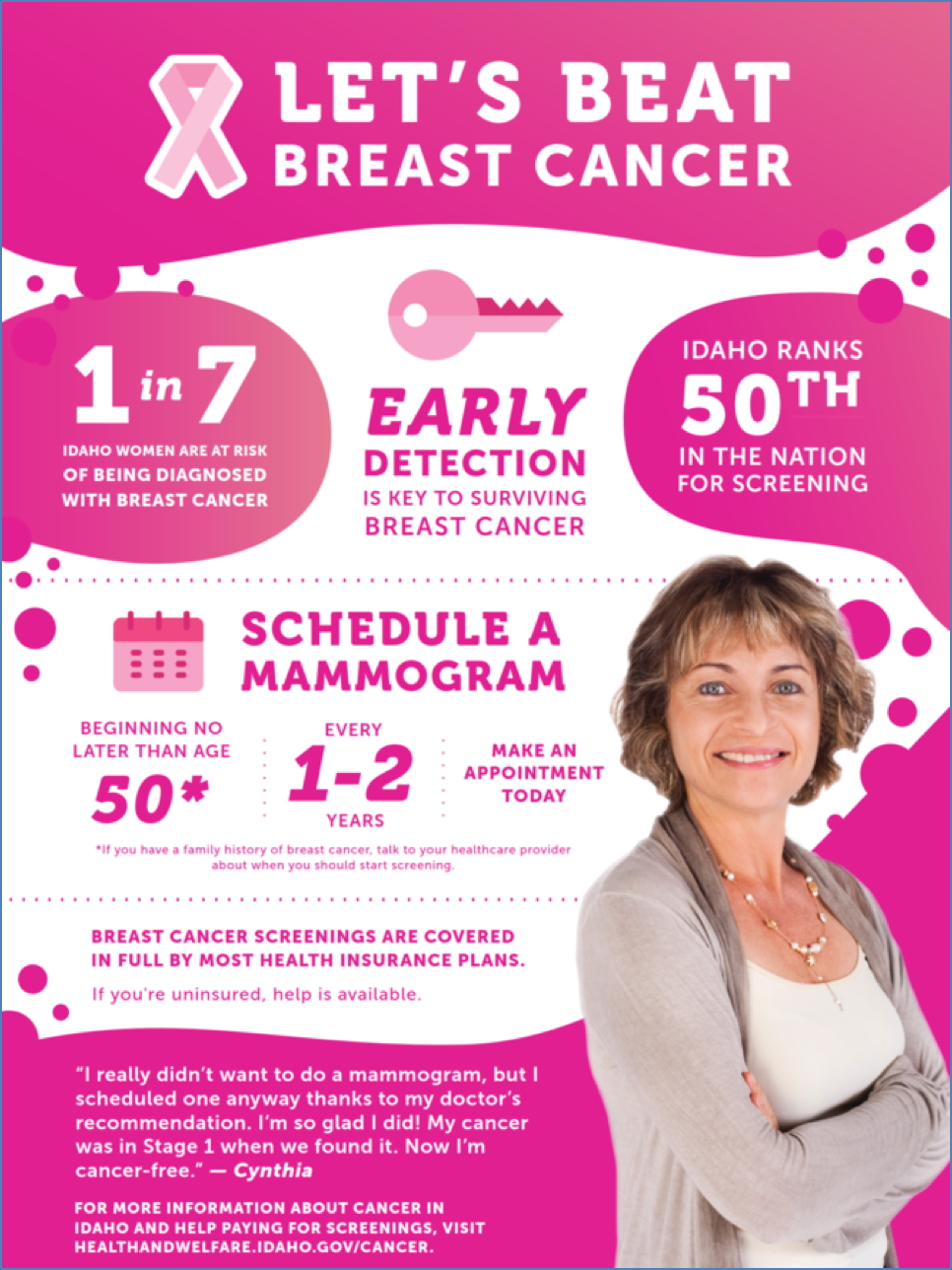
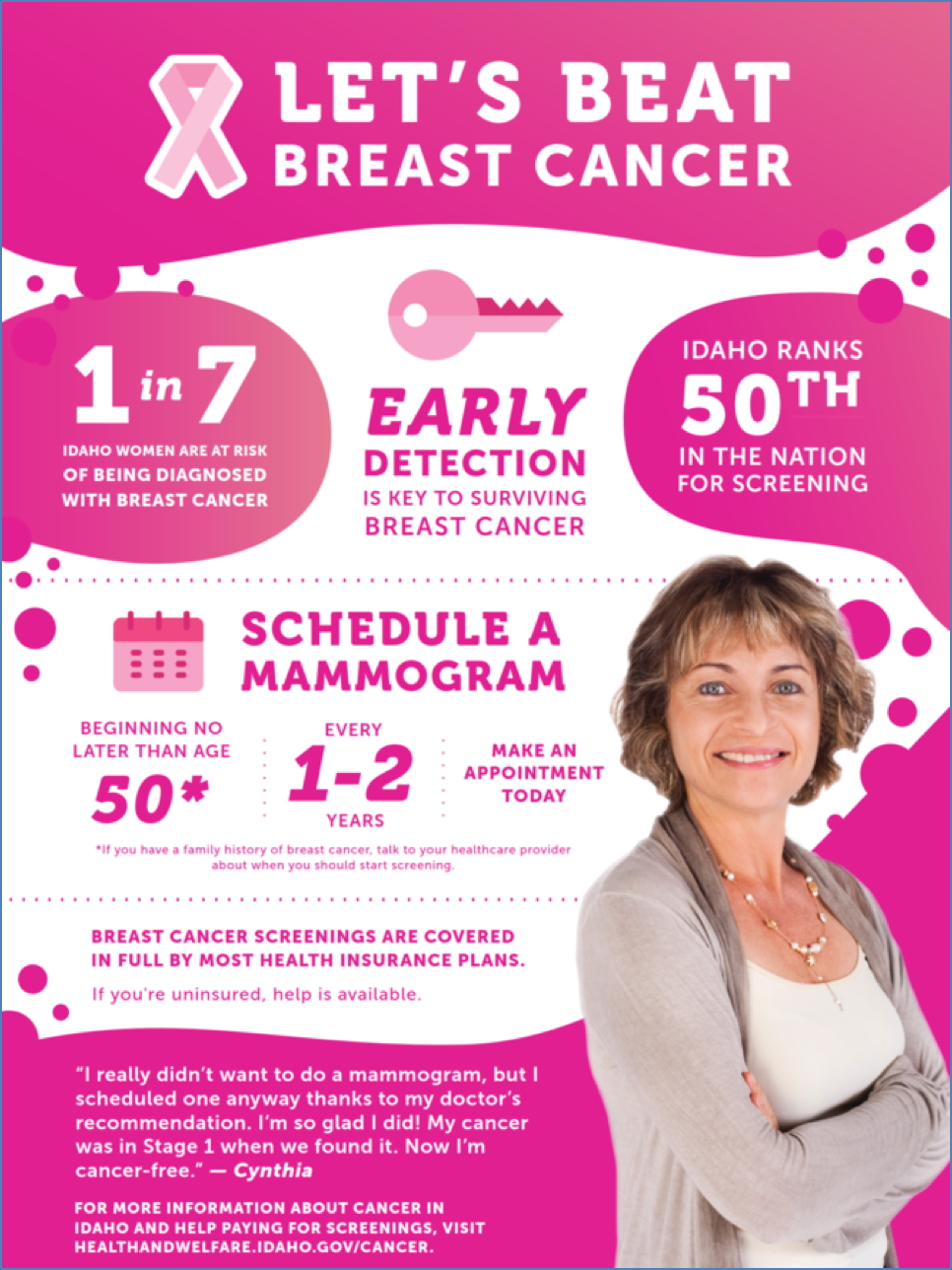
- Breast Cancer: Biennial screening >50 years
- Cervical Cancer: Pap smear + HPV immunisation
- Obesity: Annual BP, lipids, diabetes screening; nutrition checks 6-monthly
- Alcohol: 2 alcohol-free days/week
- Falls in Elderly: Vision, balance, medications, safety modifications
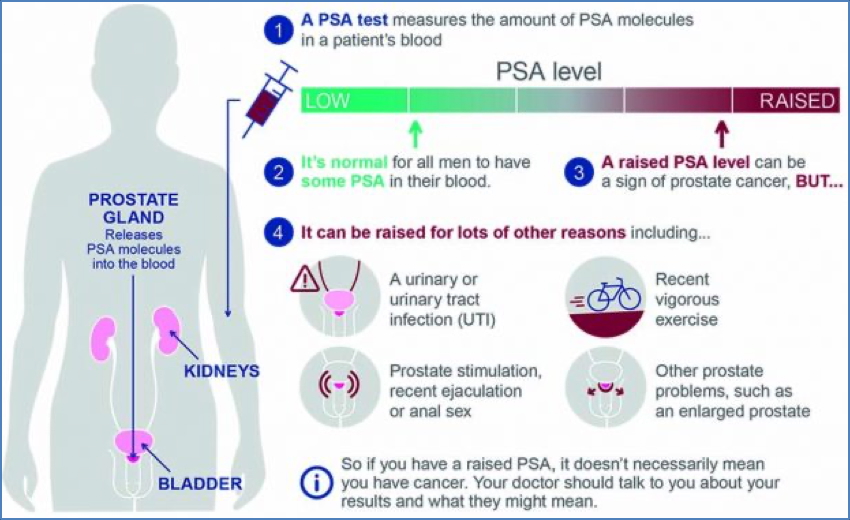
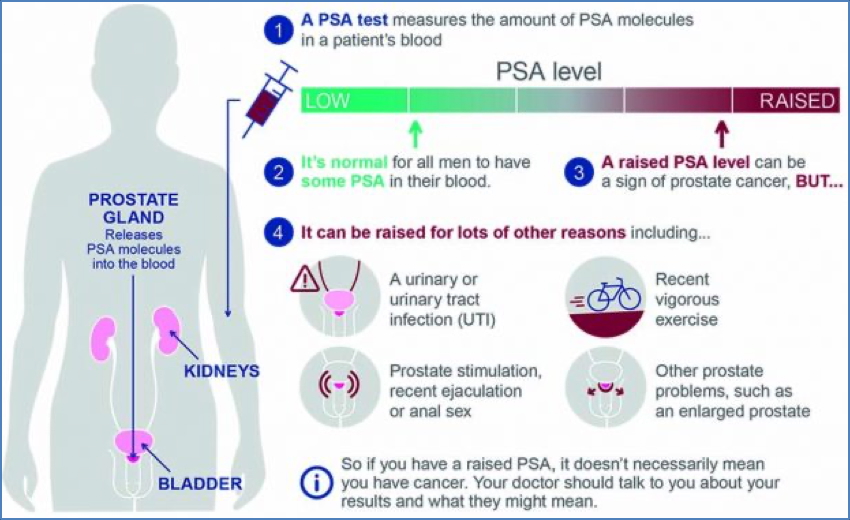
- Prostate Cancer:
- Risk: Age >50, family history, race
- Screening: Digital Rectal Exam, PSA
- Limitations: False positives, low specificity, overtreatment risks
- Management: Watchful waiting, surgery, radiation, hormone therapy
- Side effects: Incontinence, impotence, radiation effects
- Cardiovascular Risk: Use validated risk calculators












Disease Prevention Success Stories
- Vaccination – Smallpox eradication, control of measles and tetanus
- Car Safety – Seat-belts, helmets, better road design
- Workplace Safety – Reduced occupational illnesses/injuries
- Communicable Disease Control – Clean water, antibiotics, vector control
- Cardiovascular Disease – BP management, smoking cessation
- Food Safety – Pasteurisation, food fortification, safety legislation
- Maternal and Infant Health – 90%+ mortality reduction
- Water Fluoridation – 60% fewer cavities in children
- Anti-Smoking Laws – Smoking halved via policy and education
Summary – Public Health Overview
This public health overview highlights essential strategies for disease prevention, population health, and screening practices that underpin modern healthcare systems. Understanding the definitions, prevention types, and real-world applications is vital for final-year medical students. For a broader context, see our Microbiology & Public Health Overview page.