Table of Contents
Overview – Immunodeficiency
Immunodeficiency refers to a failure of the immune system to mount an adequate defence against infection. It can be primary (genetic/intrinsic) or secondary (acquired), leading to an increased risk of infections—often unusual, severe, or recurrent. Recognising signs of immunodeficiency is vital in diagnosing underlying conditions such as primary immunodeficiencies (PIDs) or HIV, and initiating appropriate therapy to prevent complications.
Definition
- A condition in which host immune defences are defective, leading to increased infection susceptibility.
- Two major types:
- Primary Immunodeficiency (PID) → Inherent/genetic immune defects
- Secondary Immunodeficiency (SID) → Acquired from external causes (infection, therapy, malnutrition)
Classification
Primary Immune Deficiency (PID)
- Genetic defects in immune function
- Often detected in infancy or early childhood
Secondary Immune Deficiency (SID)
- Caused by external insults:
- Physical: e.g. radiation
- Chemical: e.g. corticosteroids, immunosuppressive drugs
- Infective: e.g. HIV


Red Flags for Immunodeficiency
History
- Recurrent or severe infections
- Infections with unusual organisms (e.g. Pneumocystis, Serratia)
- Infections at unusual sites (e.g. nail beds)
- Predisposing events:
- Malnutrition, vitamin A deficiency
- Viral infections (e.g. HIV, measles)
- Immunosuppressive therapy
- Autoimmune disorders
- Splenectomy or other surgeries (e.g. tonsillectomy)
Examination
- Syndromic clues:
- Down’s Syndrome
- DiGeorge Syndrome
- Ataxia Telangiectasia
- Kwashiorkor
- Skin findings:
- Eczema, petechiae (e.g. Wiskott-Aldrich)
- Telangiectasia (Ataxia Telangiectasia)
- Oculocutaneous albinism (Chediak-Higashi)
- Chronic dermatitis (Hyper-IgE syndrome)
- Extensive molluscum, candidiasis (T-cell defects)
- Other signs:
- Absent tonsils
- No lymphadenopathy in the face of infection
- Poor nutritional state
- Gingivostomatitis
Investigations
- FBC with differential
- WCC morphology: Lymphocyte subsets (B cells, T cells, NK cells)
- Immunoglobulin levels (IgG, IgA, IgM)
- Antibody responses (e.g. post-vaccine titres)
- Complement levels
- Phagocytic function tests: Adhesion, oxidative burst assays
- Skin testing for delayed hypersensitivity
- Genetic testing: Identify known mutations associated with PID
Clinical Categories of Immunodeficiency
B-Cell Disorders
→ Recurrent infections with extracellular bacteria
- IgG or IgA deficiency
- Bruton’s X-linked agammaglobulinaemia (XLR)
- Common Variable Immune Deficiency – dysfunctional antibodies
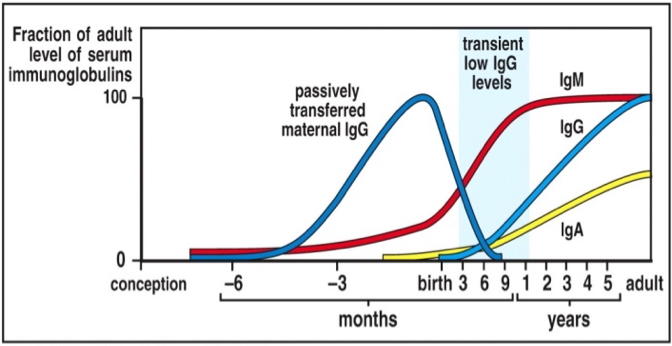
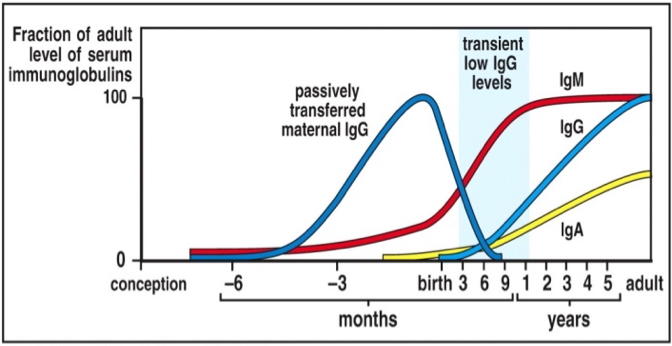
- Transient Hypogammaglobulinaemia of Infancy (THI) – temporary IgG dip at 6–12 months
T-Cell Disorders
→ Viral, fungal, and opportunistic infections
- Often combined with B-cell dysfunction
- DiGeorge Syndrome (thymic hypoplasia)
- Hyper-IgM Syndrome (isotype switching failure)
- Cytokine defects (production/receptor mutations)
Combined B- and T-Cell Disorders
→ Life-threatening infections in early life
- SCID (Severe Combined Immunodeficiency) – often X-linked
Phagocytic Dysfunction
→ Poor local infection control, chronic abscesses
- Leukocyte Adhesion Deficiency
- Chronic Granulomatous Disease – impaired killing
Complement Deficiencies
→ Poor humoral immunity, chronic infections
- Classical Pathway defects (e.g. C2, C3, C5–C9)
- Alternative Pathway defects (e.g. properdin)
- C1 esterase inhibitor deficiency → hereditary angioedema
Secondary Immunodeficiency
HIV/AIDS
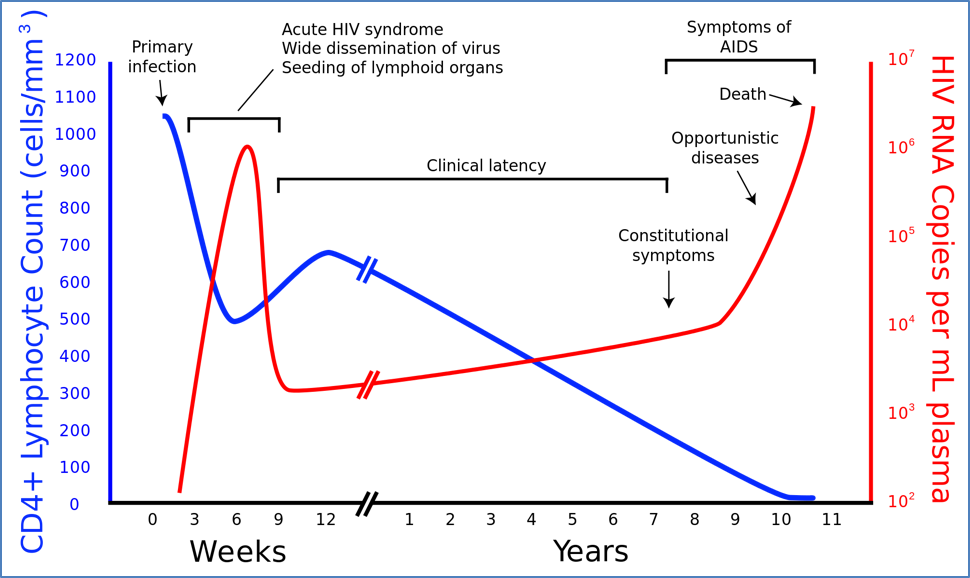
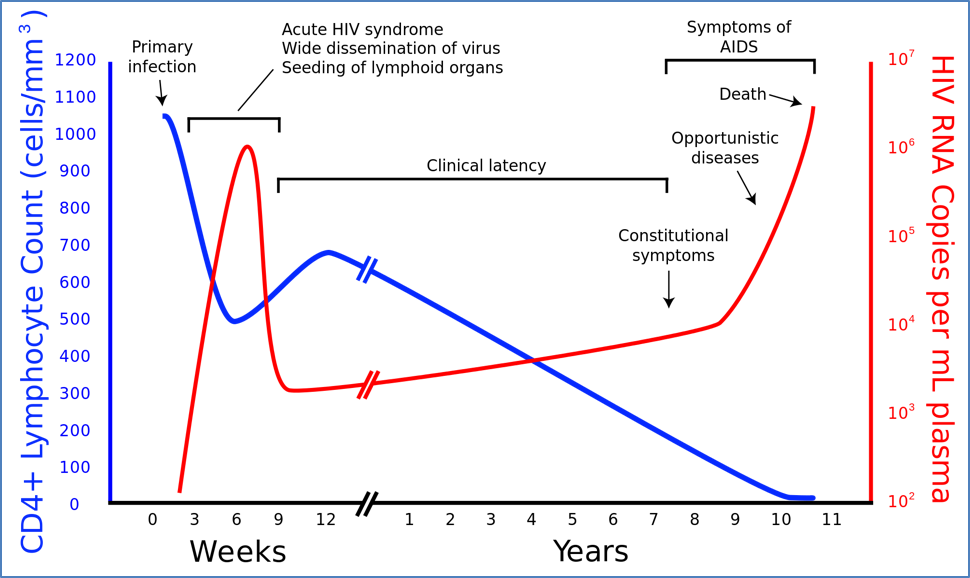
- HIV targets CD4+ T cells → loss of cell-mediated immunity
- Mechanisms:
- Cytotoxic killing of infected CD4+ cells by CD8+ cells
- Enhanced apoptosis
- HIV life cycle:
- Viral RNA → DNA (via reverse transcriptase)
- Integrated into host genome via integrase
- Dormant in memory T cells
Natural History of HIV
- Acute seroconversion illness
- Asymptomatic HIV (CD4 >500)
- Early symptomatic HIV
- Middle symptomatic HIV (CD4 200–400)
- Late symptomatic HIV (CD4 <200)
- Advanced HIV disease
Other Causes
- Malnutrition
- Immunosuppressive drugs (e.g. steroids, chemotherapy)
- Splenectomy
Management
B-Cell Deficiency
- Antibiotics
- IV immunoglobulin replacement
T-Cell / Combined Deficiencies
- Quarantine
- Prophylactic antimicrobials
- Bone marrow transplant
- Thymic transplant (e.g. DiGeorge)
Phagocyte Defects
- Antibiotics
- Bone marrow transplant
Complement Deficiency
- Plasma infusions
- Treat infections
Secondary Immunodeficiencies
- Prevention of exposure
- Aggressive infection treatment
- Antiretroviral therapy (in HIV)
Summary – Immunodeficiency
Immunodeficiency describes a failure of the immune system to protect against infection. Primary immunodeficiencies are usually genetic and appear early in life, whereas secondary forms are acquired through factors like HIV, malnutrition, or immunosuppressive therapy. Key clinical clues include unusual infections, syndromic associations, and abnormal immune markers. Management depends on the type and severity, ranging from immunoglobulin replacement to antiretroviral therapy. For a broader context, see our Immune & Rheumatology Overview page.