Table of Contents
Overview – Diverticulosis and Diverticulitis
Diverticulosis and diverticulitis are closely related gastrointestinal conditions affecting the large bowel, especially in older adults. Diverticulosis refers to the formation of diverticula (outpouchings of the bowel wall), often due to increased intraluminal pressure and age-related weakening of the colonic wall. When these pouches become inflamed or infected, the condition progresses to diverticulitis. While many individuals remain asymptomatic, complications such as bleeding, abscess formation, or perforation can pose serious health risks. Recognising this progression and treating accordingly is critical in primary care and emergency settings.
Definition
- Diverticulosis = Presence of diverticula (outpouchings) in the colonic wall
- Diverticulitis = Inflammation of one or more diverticula
Aetiology
- Acquired Causes:
- Straining during defecation
- Chronic constipation
- Age-related changes in colonic wall structure
- Congenital:
- Meckel’s diverticulum (true diverticulum)
Pathophysiology
- Diverticulosis:
- Weakening of intestinal wall + ↑ intraluminal pressure → mucosal herniation through muscularis layer
- Diverticulitis:
- Obstruction of diverticular neck by faeces → stagnation → bacterial overgrowth → localised inflammation
- May progress to perforation, abscess, or peritonitis
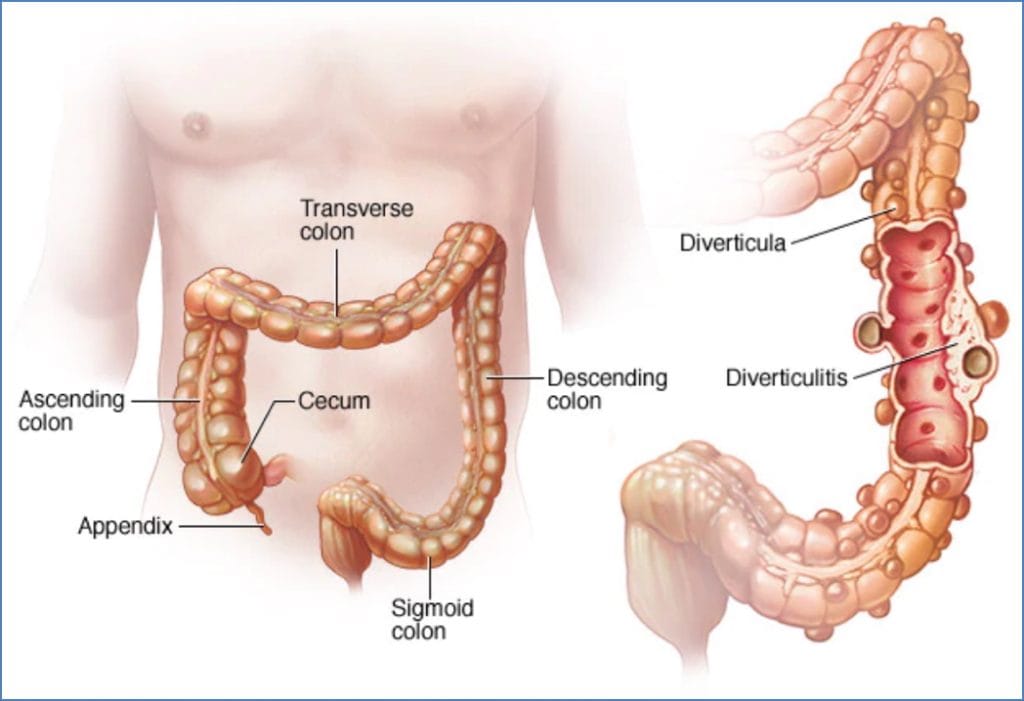
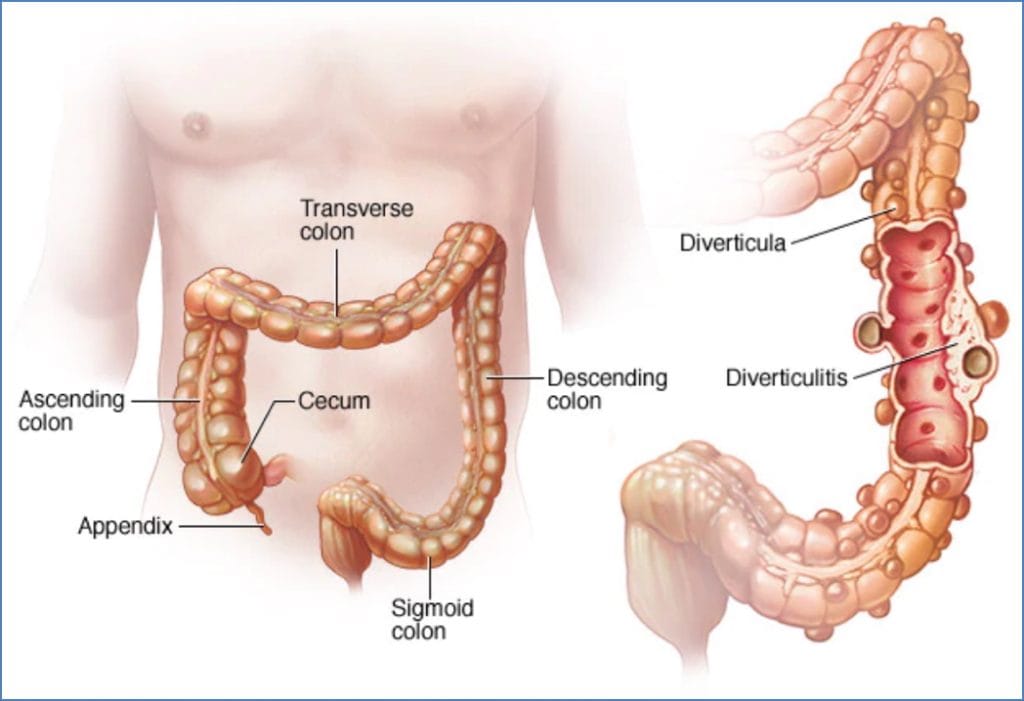
Morphology
- Herniated mucosal pouches (diverticula)
- Typically located in the left iliac fossa (LIF)


Clinical Features
- Diverticulosis:
- 95% asymptomatic
- May present with painless rectal bleeding
- Intermittent LIF pain, altered bowel habits
- Diverticulitis:
- Severe LIF pain (like appendicitis, but on the left)
- Fever, tachycardia
- If complicated → peritonitis, sepsis
Investigations
- Colonoscopy – useful in diagnosis (avoid during acute inflammation)
- FBC – leukocytosis
- Additional:
- CRP, blood cultures if febrile
- CT abdomen if complicated or atypical presentation
Management
- Lifestyle
- High fibre diet for prevention and after recovery
- Diverticulosis (asymptomatic or mild):
- Diet modification
- Non-perforated Diverticulitis:
- Broad-spectrum antibiotics:
- Ampicillin
- Gentamicin
- Metronidazole
- Broad-spectrum antibiotics:
- Perforated Diverticulitis:
- As above + surgical intervention
Complications
- Rectal bleeding – most common
- Perforation → generalised peritonitis and sepsis
- Abscess formation
- Fistulae – e.g. to bladder or vagina
- Strictures and obstruction (in chronic cases)
Summary – Diverticulosis and Diverticulitis
Diverticulosis and diverticulitis are common gastrointestinal conditions, particularly in older adults with low-fibre diets and chronic constipation. While diverticulosis is usually silent, progression to diverticulitis can lead to significant morbidity including perforation, bleeding, and sepsis. Management includes antibiotics, lifestyle changes, and surgery in severe cases. For related topics, see our Gastrointestinal Overview page.