Table of Contents
Overview – Hip Examination
The hip examination is a fundamental component of musculoskeletal and orthopaedic OSCE stations. It is essential for assessing causes of hip pain, reduced mobility, trauma, or suspected joint pathology such as osteoarthritis or fractures. A structured approach ensures that critical signs such as limb shortening, deformity, or gait abnormalities are not missed. This guide outlines a step-by-step method to perform a high-yield, clinically relevant hip examination for OSCEs and ward assessments.
Definition
A hip examination is a systematic assessment of the hip joint, soft tissues, and associated neurovascular structures. It evaluates pain, range of motion, leg alignment, muscle strength, and signs of joint pathology such as trauma, infection, or degenerative changes.
Preparation
- Wash hands, introduce yourself, confirm patient name and age.
- Explain your role and the procedure; obtain consent.
- Position: Patient supine, shorts worn, one pillow under head.
- Check surroundings: walking aids, medications (e.g. steroids) — steroids are a red flag for avascular necrosis.
Inspection
SSSS RAB Mnemonic
- Symmetry between both legs
- Swelling (inflammatory or traumatic)
- Scars (hip replacement, arthroscopy)
- Shortened leg with externally rotated foot → suggests neck of femur (NOF) fracture
- Redness (septic arthritis, inflammation)
- Atrophy of thigh or gluteal muscles
- Bruising (e.g. after trauma)
Posture & Pelvis
- Lumbar lordosis (gap between lumbar spine and bed): may suggest fixed flexion deformity
- Pelvic tilt via ASIS (anterior superior iliac spine):
- Adduction deformity: ASIS higher → limb appears shortened
- Abduction deformity: ASIS lower → limb appears lengthened
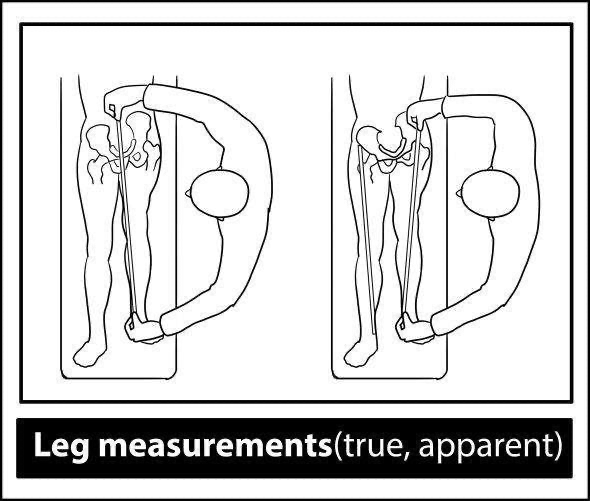
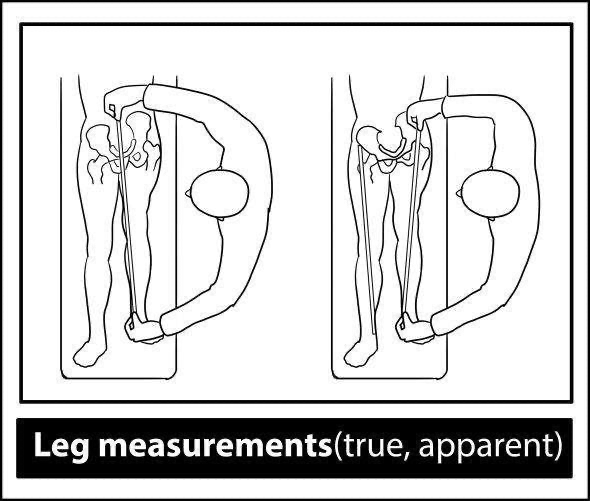
Leg Length Measurement
- Apparent length: umbilicus → medial malleolus
- True length: ASIS → medial malleolus
→ True shortening may indicate NOF fracture, dislocation, osteoarthritis, or slipped upper femoral epiphysis (SUFE)
Palpation
- Temperature over greater trochanter and hip joint (use back of hand)
- Tenderness:
- Deep hip joint (hard to localise)
- Greater trochanter → bursitis
- ASIS → insertion site of sartorius
- Vascular Sign of Narath: ↓ femoral pulse in posterior hip dislocation
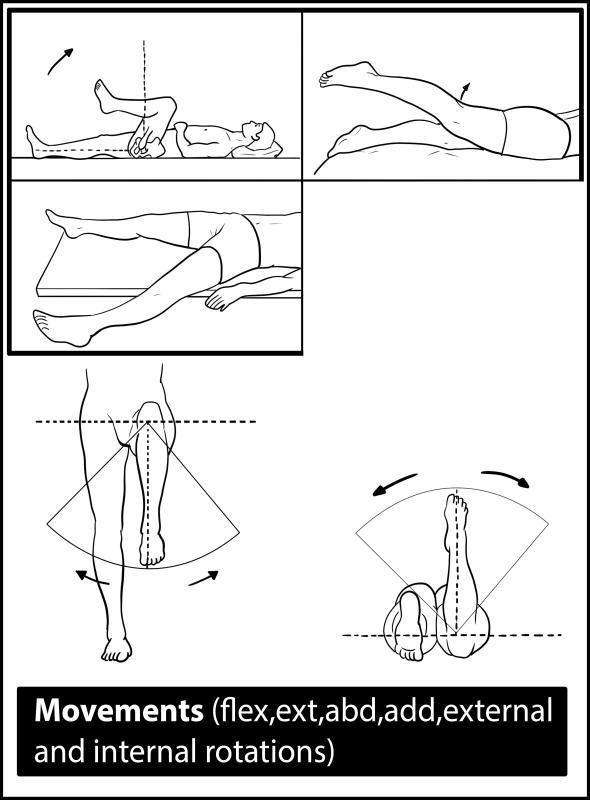
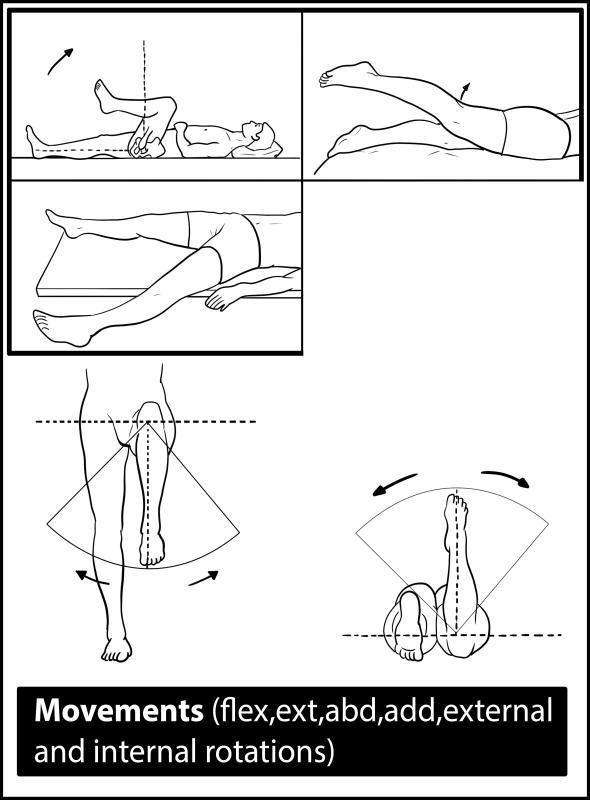
Range of Motion
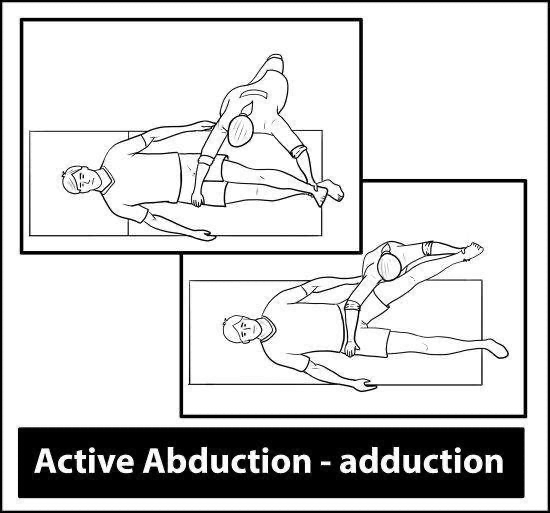
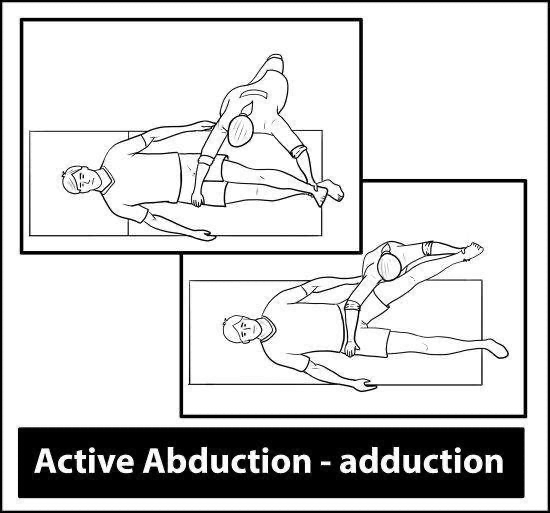
Compare active and passive range of motion (stabilise opposite pelvis during adduction/abduction):
| Movement | Normal Range | Primary Muscle(s) |
|---|---|---|
| Flexion | 120° | Iliopsoas |
| Extension | 10° | Gluteus maximus |
| Abduction | 45° | Gluteus medius and minimus |
| Adduction | 30° | Adductor group |
| External Rotation | 40° | Obturators, quadratus femoris, gemelli |
| Internal Rotation | 40° | Iliopsoas |
Reduced internal rotation is often an early sign of osteoarthritis.
Special Tests
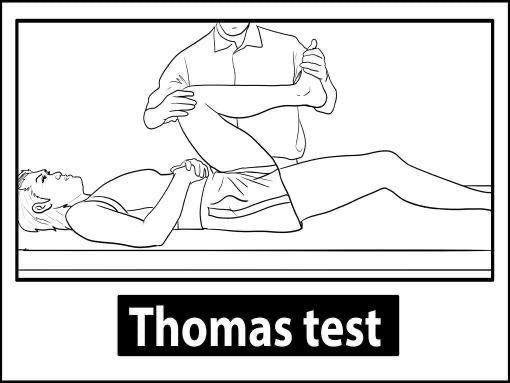
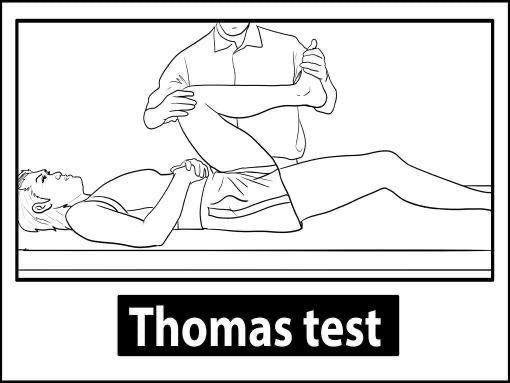
Thomas Test – Fixed Flexion Deformity
- With patient supine, place hand under lumbar spine.
- Ask patient to flex one hip toward chest.
- Positive = opposite thigh lifts off the table → indicates fixed flexion deformity.
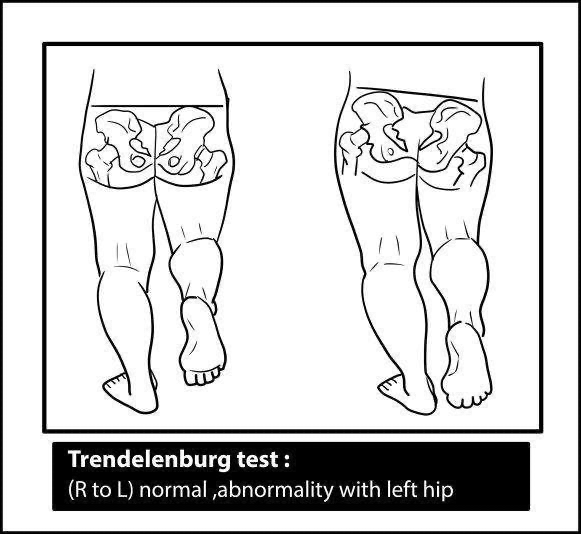
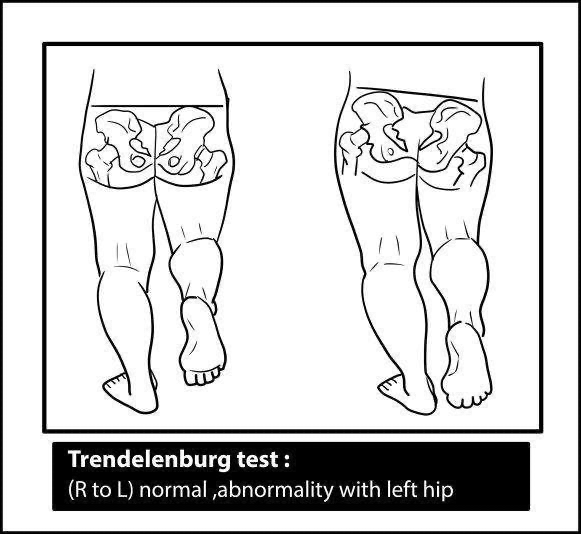
Trendelenburg Test – Gluteus Medius Weakness
- Patient stands on one leg.
- Positive = pelvis drops on lifted leg → weak contralateral gluteus medius/minimus (superior gluteal nerve injury).
- Causes: dislocation, OA, muscle weakness, hip dysplasia.
Standing Assessment
- Inspect spinal alignment – scoliosis may indicate fixed abduction/adduction deformities.
- Gluteal atrophy – often seen in hip OA.
- Gait patterns:
- Antalgic gait – shortened stance phase (painful hip)
- Waddling gait – bilateral abductor weakness
Clinical Correlations
Hip Fractures
Intracapsular (above intertrochanteric line)
- E.g. Neck of femur fractures
- Risk: Elderly (osteoporosis), falls
- Signs: Shortened, externally rotated leg, ↓ ROM
- Classification: Garden I–IV
- Treatment:
- Young: ORIF (open reduction internal fixation)
- Elderly: Hemiarthroplasty or total hip replacement (THR)
Extracapsular
- Includes intertrochanteric and subtrochanteric fractures
- Treatment: Internal fixation (dynamic hip screw)
Complications: Avascular necrosis, non-union, thromboembolism, fat embolism
Hip Dislocation
- Posterior: Most common. May damage sciatic nerve.
- Anterior: Rare. May damage femoral nerve.
Osteoarthritis (OA)
- Common joints: Hip, knee, DIP, PIP, spine
- Risk factors: Age, obesity, trauma, rheumatoid arthritis
- Symptoms:
- Pain/stiffness worsens with use
- ↓ROM
- Flexion/adduction deformities
- Crepitus
- X-ray (LOSS):
- Loss of joint space
- Osteophytes
- Subchondral sclerosis
- Subchondral cysts
- Management:
- Weight loss
- Paracetamol or NSAIDs (±PPI)
- Intra-articular steroids (e.g. triamcinolone)
- Total hip replacement if severe
Osteoporosis
- Features: Low bone density → ↑ fracture risk
- Risk factors: Age, female, low BMI, steroids, menopause
- Investigations: DEXA scan
- T-score:
- −1.0 to −2.5 = osteopenia
- ≤ −2.5 = osteoporosis
- T-score:
- Treatment:
- Bisphosphonates
- Calcium & vitamin D
- Denosumab, estrogen (selectively)
Differential Diagnosis of Hip Pain
- OA, RA
- Septic arthritis
- Bursitis
- Muscle strain
- Referred pain from lumbar radiculopathy
Summary – Hip Examination
The hip examination is essential for diagnosing joint, nerve, or musculoskeletal pathology in clinical and OSCE settings. By assessing inspection findings, leg length, joint mobility, and performing key special tests like Thomas and Trendelenburg, clinicians can identify conditions such as hip fractures, dislocations, osteoarthritis, and more. For a broader context, see our OSCE Prep Overview page.