Table of Contents
Overview – Blood and Immunity
Blood and immunity are intrinsically linked — the immune system is dynamic, and reliant on immune cells and signalling molecules transported via the blood and lymph. From circulating granulocytes and lymphocytes to cytokines and antibodies, blood plays a central role in immune surveillance, pathogen elimination, and inflammation. This overview focuses on the haematological side of immune defence, with more detailed immunopathology and autoimmune topics covered in the Immune & Rheumatology section.
Definition
- The immune system is a functional system, not an organ system
- It protects the body from:
- Pathogens (bacteria, viruses, fungi)
- Cancer cells
- Transplants and grafts
- Involves cells, molecules, and cytokines found in blood and lymph
Terminology
- Pathogen: Microorganism that can cause disease
- Virulence: Degree of pathogenicity
- Opportunistic pathogen: Causes disease in immunocompromised hosts
- Normal flora: Harmless resident bacteria
- Infection: Microbial invasion of a normally sterile site
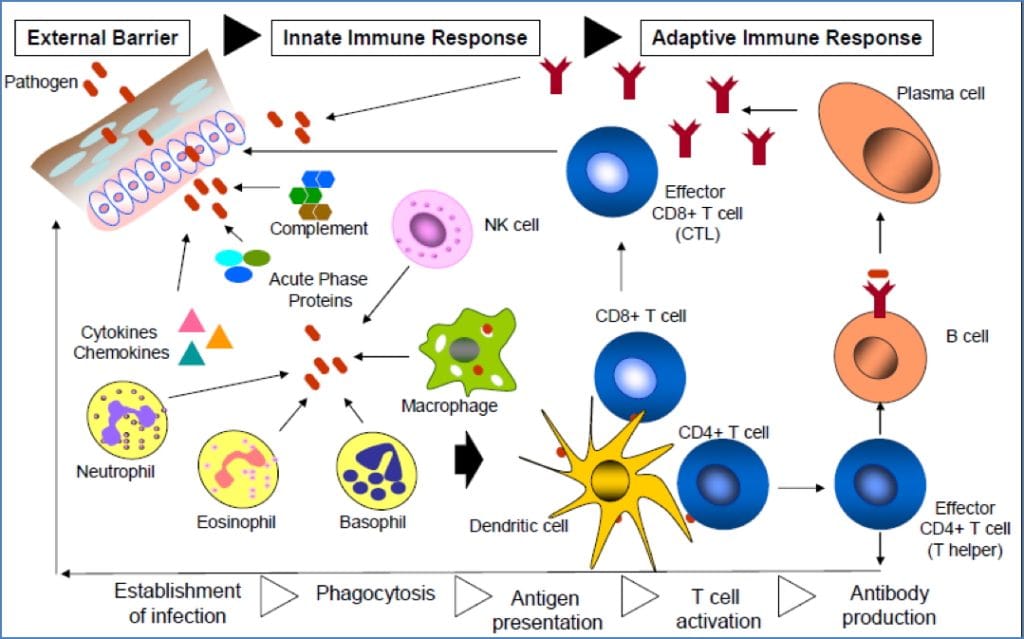
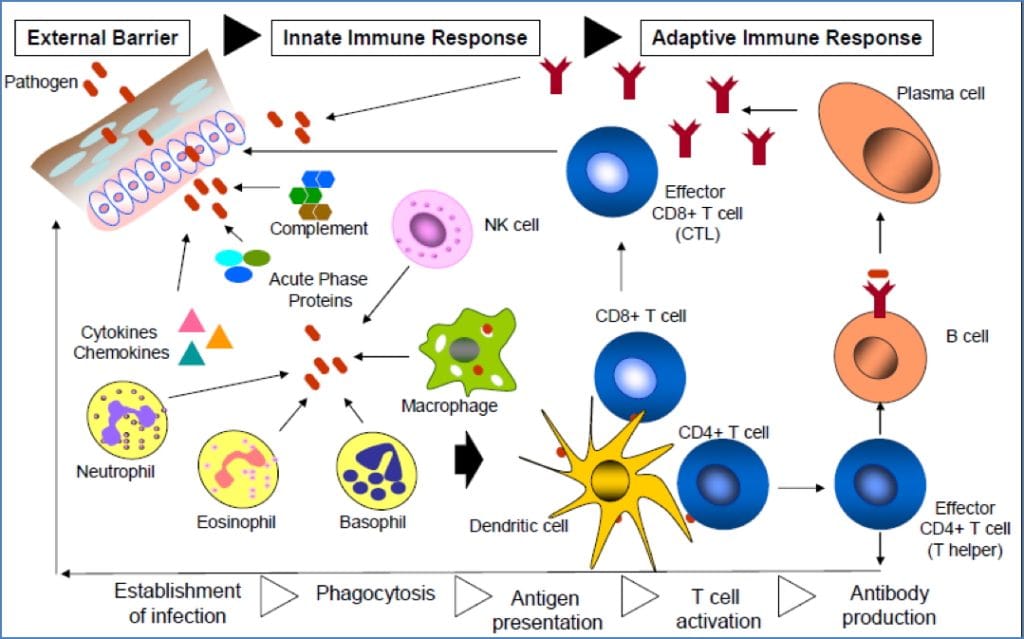
Innate Immune System (Non-Specific)
General Features
- Present at birth
- Responds within minutes
- Not antigen-specific
- Forms the first and second lines of defence
1st Line – Surface Barriers
- Skin: stratified, keratinised epithelium
- Mucous membranes: trap microbes with mucus and destroy them with:
- Lysozyme in tears/saliva
- Acidic secretions (skin, stomach, vagina)
- Cilia sweep pathogens to the digestive tract




2nd Line – Internal Defence
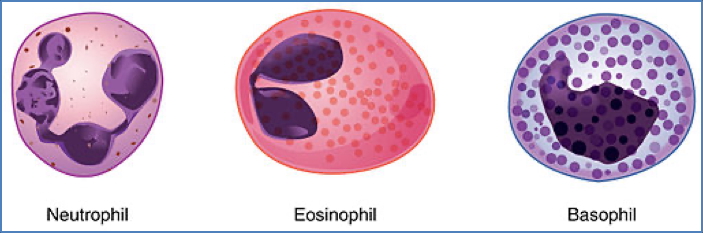
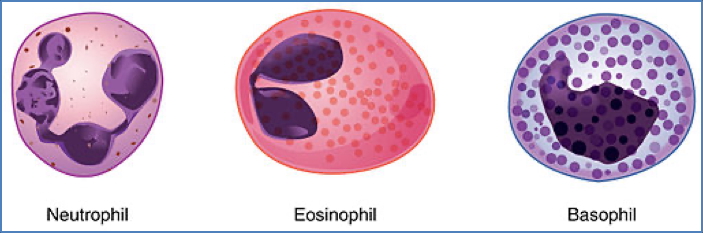
- Phagocytes:
- Macrophages: engulf pathogens and debris
- Neutrophils: phagocytic + cytotoxic granules
- Eosinophils: anti-parasitic, also present in allergy
- Basophils: histamine release in allergy


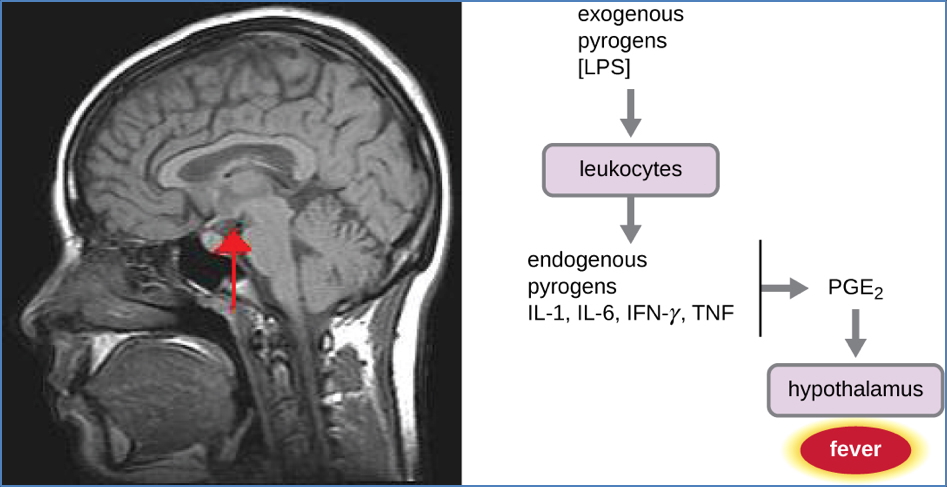
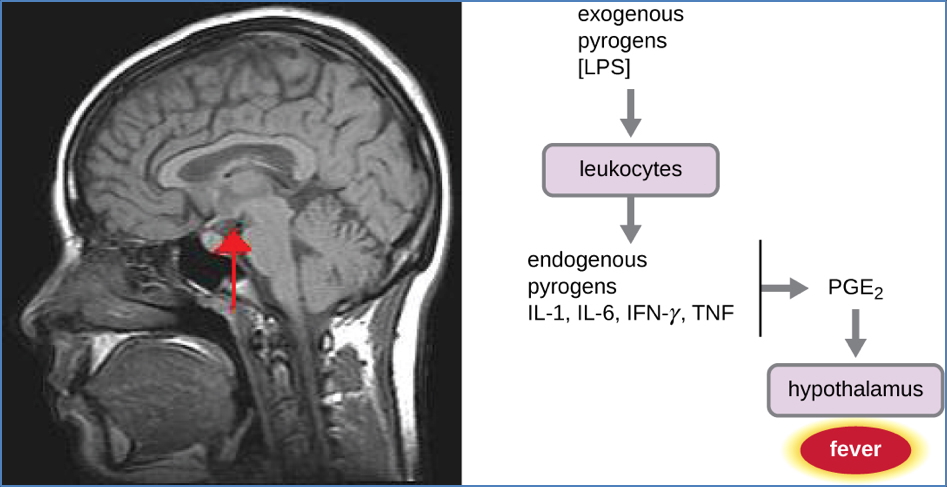
- Fever: induced by pyrogens → raises metabolism and inhibits pathogens
- Natural Killer (NK) cells:
- Detect “non-self” via absence of MHC-I
- Induce apoptosis in infected/cancerous cells
- Promote inflammation via cytokines


- Antimicrobial Proteins:
- Interferons: antiviral
- Complement proteins: opsonisation, lysis
- Inflammation:
- Triggered by trauma, heat, toxins, infection
- Hallmarks: redness, heat, pain, swelling
- Functions:
- Limit spread of injury
- Dispose of debris
- Prepare tissue for repair
Adaptive Immune System (Specific)
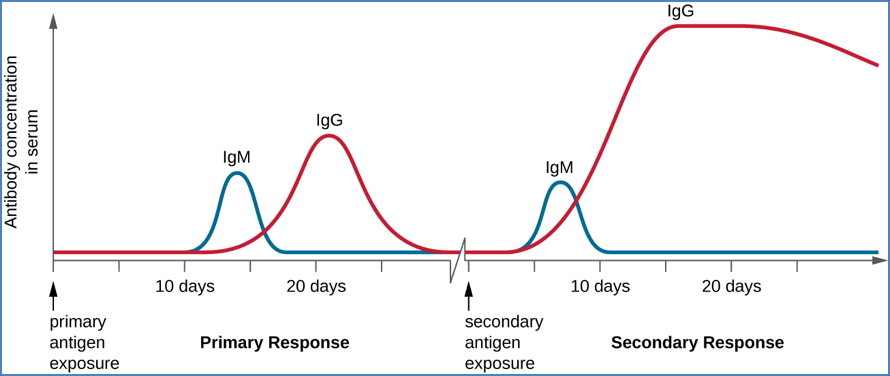
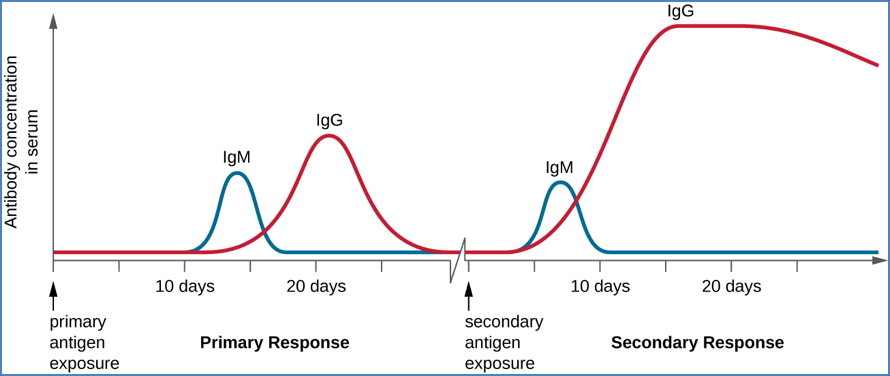
General Features
- Third line of defence
- Antigen-specific
- Systemic
- Has memory (basis of vaccines)
Cellular Immunity
- T Lymphocytes:
- Recognise infected/cancerous cells via antigen presentation
- Subtypes:
- Cytotoxic T cells: induce apoptosis
- Helper T cells: recruit and activate other immune cells
- Macrophages & NK cells:
- Destroy intracellular pathogens
- Secrete cytokines to amplify responses
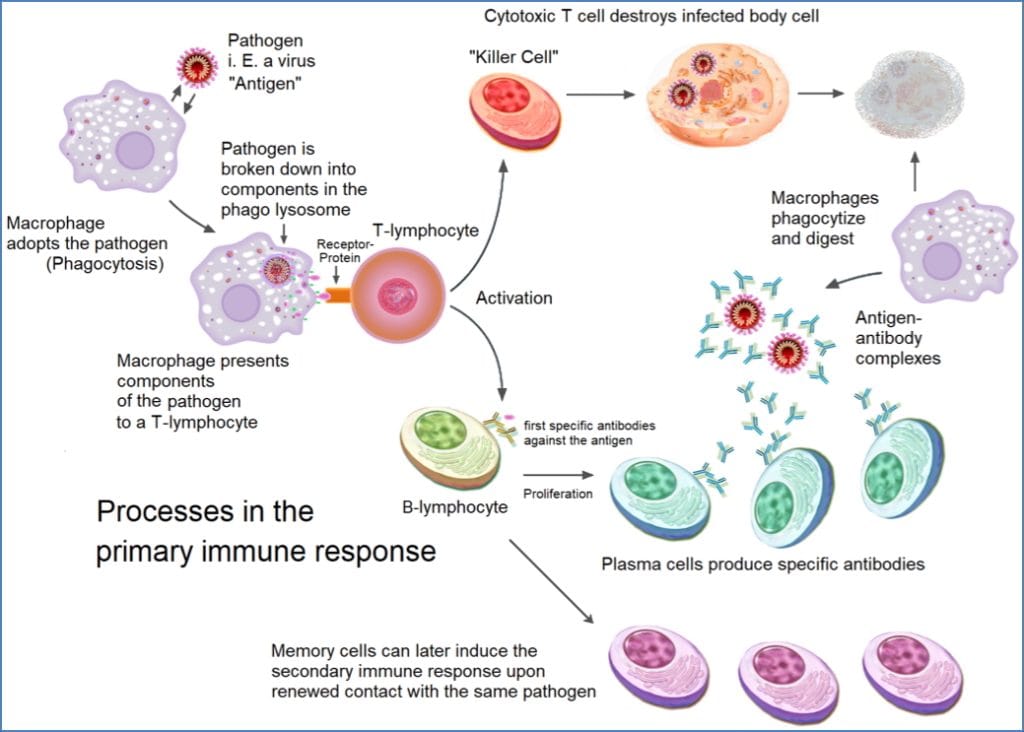
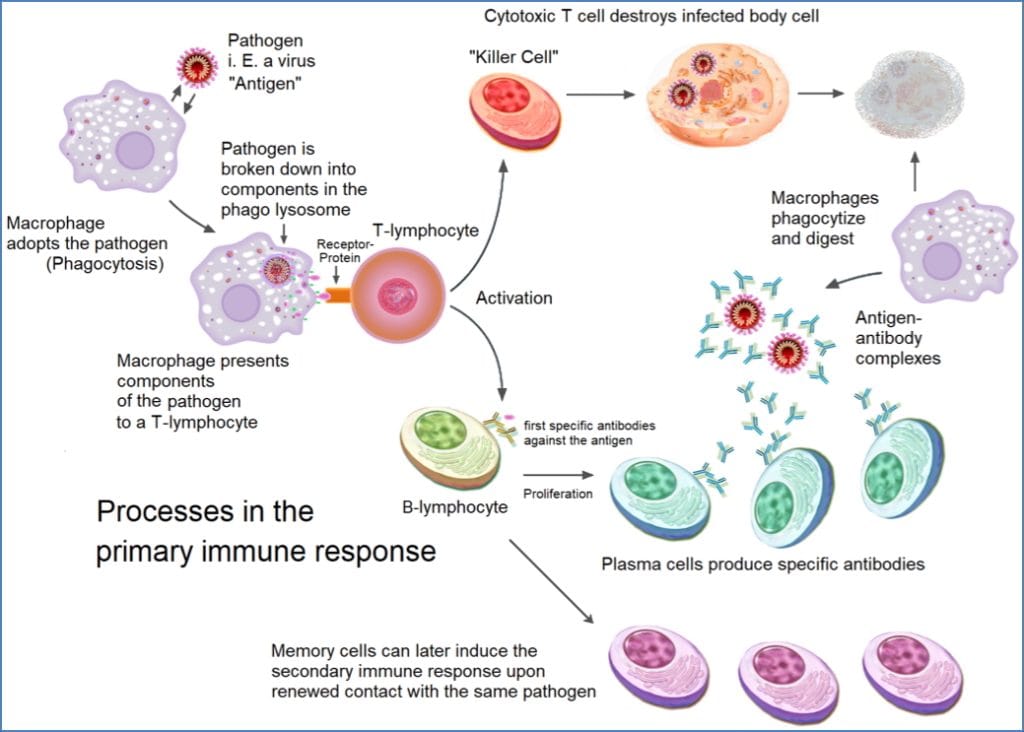
Humoral Immunity
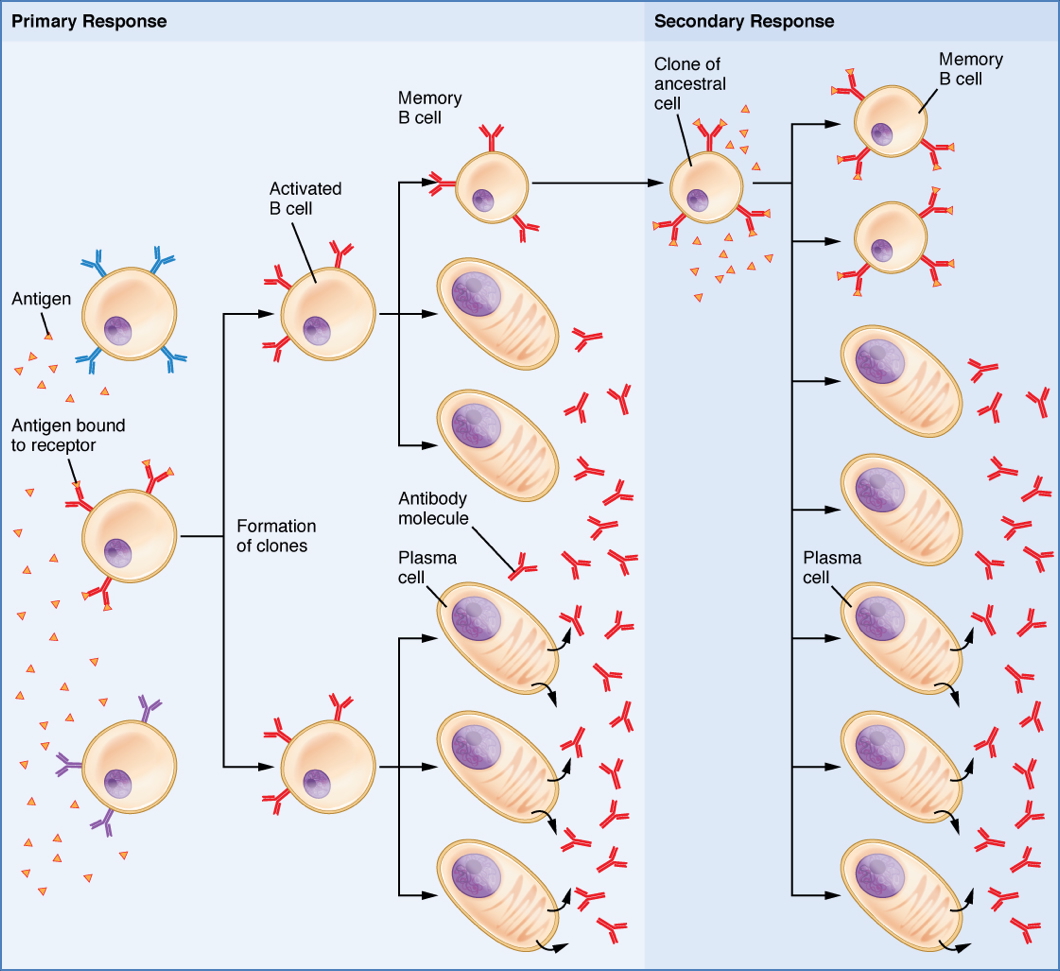
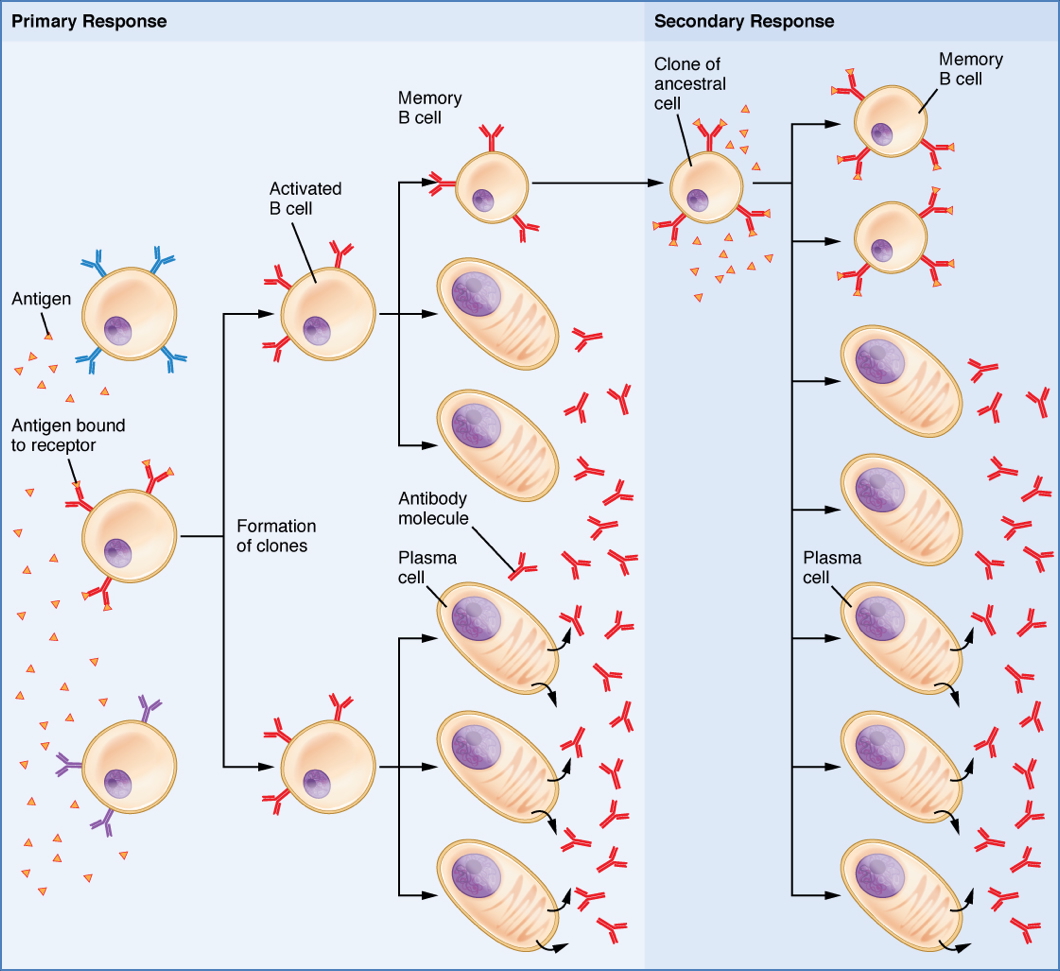
- B Lymphocytes:
- Produce antibodies (immunoglobulins)
- Antibodies bind antigens in blood/lymph → neutralisation and opsonisation
- After exposure:
- Plasma cells make antibodies
- Memory B cells provide rapid future responses
Clinical Context in Haematology
- White blood cells in blood counts reflect immune activity
- Elevated neutrophils: bacterial infection
- Elevated lymphocytes: viral infection
- Low immune cells: immunodeficiency, marrow failure, chemotherapy effect
- Monoclonal antibodies and immunomodulators are now standard haematological therapies
Summary – Blood and Immunity
Blood is central to immunity against microorganisms, acting as the transport medium for white cells, cytokines, and antibodies. Innate defences act quickly and broadly, while adaptive responses are antigen-specific and have memory. This immunological arm of haematology is essential for understanding infections, autoimmune conditions, and lymphoproliferative disorders. For a broader context, see our Blood & Haematology Overview page.

